Airgas template - PowerPoint PPT Presentation
1 / 52
Title:
Airgas template
Description:
Two Parts of the Circulatory System. Pulmonary circulation ... Explain the effect of cardiac reserve on symptom development in heart failure. ... – PowerPoint PPT presentation
Number of Views:119
Avg rating:3.0/5.0
Title: Airgas template
1
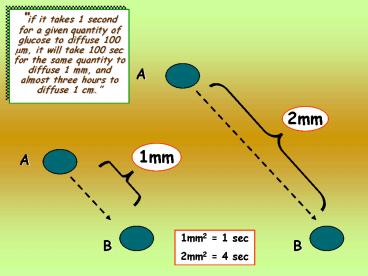
if it takes 1 second for a given quantity of
glucose to diffuse 100 ?m, it will take 100 sec
for the same quantity to diffuse 1 mm, and almost
three hours to diffuse 1 cm.
A
2mm
1mm
A
1mm2 1 sec 2mm2 4 sec
B
B
2
So, diffusion is only effective when dealing with
a large surface area, minimal thickness, and a
relatively inactive tissue
Ficks Law of Diffusion Diffusion (C1
C2) SA thickness
3
More complex body plans Diffusion fails as a
sole means of distribution
Convective Exchange (constant) ?V (C1 C2)
Campbell Fig.32.4
4
- Flow (F) Pressure Gradient (?P)
- Resistance (R)
- What is this flow transporting?
- 1. Gases
- 2. Solutes
- 3. Nutrients
- 4. Hormones (chemical messages)
- 5. Wastes
- 6. Heat
- 7. Force
How do you get a good pressure gradient?
5
http//yakko.bme.virginia.edu/lab/images/beating_h
eart.gif
6
Gradual separation of the heart into two separate
pumps
7
Two Parts of the Circulatory System
- Pulmonary circulation
- Moves blood through the lungs and creates a link
with the gas exchange function of the respiratory
system - Systemic circulation
- Supplies all the other tissues of the body
Body
Lungs
Right Heart
Left Heart
8
The Heart as a Pump
- The heart is an intermittent pump
- Blood flow in the arterial circulation is
pulsatile
Porth Fig. 23.2
9
Moyes and Schulte Figure 9.31
10
GEOMETRY OF BLOOD VESSELS IN DOG MESENTERY
11
- Poiseuilles law
Porth Fig. 23.3
12
Usually the major determinant of TPR
http//www.oucom.ohiou.edu/CVPhysiology/H003.h
tm
13
Resistance varies inversely with the fourth power
of the vessel
R 1 r4
so, if the radius of a vessel is doubled, the
resistance drops to 1/16th of its original value
r4 1 x 1 x 1 x 1 1
r4 2 x 2 x 2 x 2 16
http//nobelprize.org/medicine/laureates/1998/meda
nim/images.html
14
Atherosclerotic plaque forming in a coronary
artery.
. decreasing radius (r), and increasing
resistance
. which is made even worse if a spasm develops
in the wall of this vessel
15
So, if a drug can be provided that relaxes the
spasm.
radius will be increased, and resistance will
be lessened
and flow will be increased
16
Velocity
Inversely proportional to cross-sectional area
Porth Fig. 23.4
17
- Blood pressure is highest in the left ventricle
- Blood pressure drops rapidly in arterioles due to
high resistance - Blood pressures decreases as the blood moves
through the system - The velocity of blood is highest in the arteries
(high pressure), lowest in the capillaries (large
cross-sectional area), and intermediate in the
veins (lower pressure and cross-sectional area)
Moyes and Schulte Figure 9.33
18
Laminar vs. Turbulent Flow
Porth Fig. 23.5
V 1 r2
http//user.icx.net/richmond/heartAS1795a.jpg
19
Law of LaPlace (1) Pressure depends upon
surface tension and radius (a) P 2T/r
http//www.pathguy.com/lectures/aortic_aneurysm.jp
g
Porth Fig. 23.5
20
Compliance and elastance
- a) Compliance ( ? V / ? P)
- (1) ability to stretch
- b) Elastance
- (1) ability to return to original position
21
(No Transcript)
22
(No Transcript)
23
24
25
Preload, afterload, and contractility
Porth Fig. 23.16
- Preload amount of tension on the muscle before
it contracts - Afterload load against which the muscle exerts
its contraction - c) Contractility changes in stroke volume not
attributable to either preload or afterload
(increase in the strength of contraction without
an increase in length)
26
SV EDV - ESV
EDV
Aortic pressure or mean arterial pressure
Powers and Howley Page 257
27
Powers and Howley Page 255
28
(No Transcript)
29
(No Transcript)
30
(No Transcript)
31
Regulation of Circulatory Systems
- CO MAP/TPR
32
Baroreceptors
- Baroreceptors are stretch-sensitive
mechanoreceptors located in the walls of many
major blood vessels - Most important of these are located in the
carotid artery and aorta - Baroreceptor reflex regulates MAP
33
- Explain the effect of cardiac reserve on symptom
development in heart failure. - Define the terms preload, afterload, and cardiac
contractility. - Explain how increased Frank-Starling mechanism,
sympathetic activity, the renin-angiotensin-aldost
erone mechanism, the natriuretic peptides, the
endothelins, and myocardial hypertrophy and
remodeling contribute to the initial adaptation
to heart failure and then to its progression. - 4. Differentiate high-output versus low-output
heart failure, systolic versus diastolic heart
failure, and right-sided versus left-sided heart
failure.
XXXXXXX
34
- Explain the effect of cardiac reserve on symptom
development in heart failure. - Page 604 The heart has an amazing capacity to
adjust its pumping ability to meet the varying
needs of the body. During sleep its output
declines, and during exercise, it increases
markedly. The ability to increase cardiac output
during increased activity is called cardiac
reserve.
35
- Define the terms preload, afterload, and cardiac
contractility. - Page 604 Preload reflects the loading
condition of the heart at the end of diastole
just before the onset of systole. It is the
volume of blood stretching the resting heart
muscle and is determined mainly by venous return
to the heart. For any given cardiac cycle, the
maximum volume of blood filling the ventricle is
present at the end of diastole. Known as the
end-diastolic volume, this volume causes the
tension in the walls of the ventricles and the
pressure in the ventricles to rise.
36
- Define the terms preload, afterload, and cardiac
contractility. - Page 604 Afterload represents the force that
the contracting heart must generate to eject
blood from the filled heart. The main components
of afterload are the systemic (peripheral)
vascular resistance and ventricular wall
tension.
37
- Define the terms preload, afterload, and cardiac
contractility. - Page 604 Cardiac contractility refers to the
mechanical performance of the heart the ability
of the contractile elements (actin and mysosin
filaments) of the heart muscle to interact with
and shorten against a load. The ejection of
blood from the heart during systole depends on
cardiac contractility. Cardiac contractility
increases cardiac output independent of preload
filling and muscle stretch.
38
- Explain how increased Frank-Starling mechanism,
sympathetic activity, the renin-angiotensin-aldost
erone mechanism, the natriuretic peptides, the
endothelins, and myocardial hypertrophy and
remodeling contribute to the initial adaptation
to heart failure and then to its progression.
XXXXXXX
39
- Explain how increased Frank-Starling mechanism,
sympathetic activity, the renin-angiotensin-aldost
erone mechanism, the natriuretic peptides, the
endothelins, and myocardial hypertrophy and
remodeling contribute to the initial adaptation
to heart failure and then to its progression.
XXXXXXX
Length-tension relationship
Page 605 The Frank- Starling mechanism
increases stroke volume by means of an increase
in end-diastolic volume.
Marieb Fig. 9.22
40
- Explain how increased sympathetic activity
contributes to the initial adaptation to heart
failure and then to its progression.
Page 606 Stimulation of the sympathetic
nervous system plays an important role in the
compensatory response to decreased cardiac output
and to the pathogenesis of heart failure. The
negative aspects of increased sympathetic
activity include an increase in systemic vascular
resistance and the afterload against which the
heart must pump.
41
- Explain how the renin-angiotensin-aldosterone
mechanism contributes to the initial adaptation
to heart failure and then to its progression.
Page 606 One of the most important effects of
a lowered cardiac output in heart failure is a
reduction in renal blood flow and glomerular
filtration rate, which leads to salt and water
retention.
42
Page 606 Because aldosterone is metabolized in
the liver, its levels are further increased when
heart failure cause liver congestion.
43
- Explain how the natriuretic peptides contribute
to the initial adaptation to heart failure.
44
- Explain how myocardial hypertrophy and
remodeling contribute to the initial adaptation
to heart failure and then to its progression. - Page 607 The development of myocardial
hypertrophy constitutes one of the primary
mechanisms by which the heart compensates for an
increase in workload. Although ventricular
hypertrophy improves the work performance of the
heart, it also is an important risk factor for
subsequent cardiac morbidity and mortality.
Symmetric hypertrophy
Concentric hypertrophy
Eccentric hypertrophy
45
4. Differentiate high-output versus low-output
heart failure, systolic versus diastolic heart
failure, and right-sided versus left-sided heart
failure. High- output and low-output heart
failure are described in terms of cardiac
output. High-output failure is an uncommon type
of failure that is caused by excessive need for
cardiac output. Low-output failure is caused by
disorders that impair the pumping ability of the
heart, such as ischemic heart disease and
cardiomyopathy.
46
Differentiate high-output versus low-output heart
failure, systolic versus diastolic heart failure,
and right-sided versus left-sided heart
failure. Page 608 Systolic heart failure
involves a decrease in cardiac contractility and
ejection fraction ischemic hear disease, volume
overload, pressure overload Page 609 Diastolic
heart failure is characterized by a smaller
ventricular chamber size, ventricular
hypertrophy, and poor ventricular compliance
mitral stenosis, hypertrophy due to lung disease.
47
Differentiate high-output versus low-output heart
failure, systolic versus diastolic heart failure,
and right-sided versus left-sided heart failure.
A weight gain of more than 2 in 24 hours or 5
in a week
48
http//www3.hku.hk/surgery/images/trc_01.jpg
49
(No Transcript)
50
http//www.dialog.samara.ru/help/images/eng/iabp.g
if
IABP
counterpul-sations
51
(No Transcript)
52
(No Transcript)