Clinical Correlation: Lung Disease - PowerPoint PPT Presentation
1 / 36
Title:
Clinical Correlation: Lung Disease
Description:
Distinct entities or disease progression. Chronic Bronchitis. Signs ... 'Barrel-chested', weight loss 'Pink puffers': pursing of lips, non cyanotic. pink puffer ... – PowerPoint PPT presentation
Number of Views:171
Avg rating:3.0/5.0
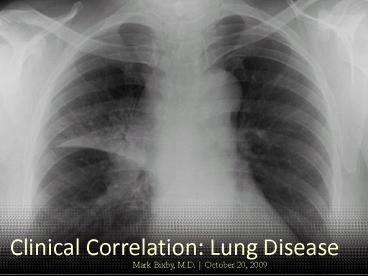
Title: Clinical Correlation: Lung Disease
1
Clinical Correlation Lung Disease
Mark Bixby, M.D. October 20, 2009
2
Lung Disease
- Chronic obstructive pulmonary disease (COPD)
- Chronic Bronchitis
- Emphysema
- Asthma
- Tuberculosis
3
Lung Disease
- Chronic obstructive pulmonary disease (COPD)
- Chronic Bronchitis
- Emphysema
4
COPD Definition
- Chronic airflow limitation not fully reversible
- Two major diseases
- Chronic bronchitis
- Emphysema
- Overlapping symptoms
- Distinct entities or disease progression
5
Chronic Bronchitis Signs and Symptoms
- Onset phase years
- Chronic cough, copious sputum
- gt3 months
- 2 consecutive years
- Blue bloaters sedentary, overweight, cyanotic,
edematous, breathless - Severity based on spirometry
6
Interpreting Spirometry - definitions
7
Severity of COPDBased on Spirometry
8
Emphysema Signs and Symptoms
- Severe exertional dyspnea, minimal cough
- Prolonged expiratory phase
- Barrel-chested, weight loss
- Pink puffers pursing of lips, non cyanotic
9
pink puffer
blue bloater
10
COPD Lab Tests
- Spirometry
- ? maximum expiratory flow rate not reversible
- Chest x-ray
- Chronic bronchitis prominent vascular markings
- Emphysema over distention of lungs, flattening
of diaphragm, emphysematous bullae
11
COPD Medical Management
- No cure, but can improve quality of life
- Early management
- Smoking cessation, ? exposure to pollutants
- Regular exercise, good nutrition, prevention of
respiratory infections, adequate hydration - Oxygen therapy when SpO2 88
- Beta agonists, anticholinergics, inhaled
corticosteroids, theophylline
12
COPD Dental Management
- Encourage quitting smoking
- Reschedule appointment if
- Short of breath worse than baseline
- Productive cough worse than baseline
- Acute upper respiratory infection
- Oxygen saturation lt91 (by pulse oximeter)
13
COPD Dental Management of Stable Patient
Things to do
- Treat in upright chair position
- Use inhalers prior to treatment
- Use pulse oximetry
- Use low-flow oxygen when O2 sat lt95 unless
baseline is lower - May use low-dose oral diazepam
- Supplemental steroids may be required
14
COPD Dental Management of Stable Patient
Things to avoid
- Rubber dam use (in severe cases)
- N2O sedation (in severe or very severe COPD)
- Barbiturates and narcotics
- Antihistamines and anticholinergics
- Macrolide antibiotics and ciprofloxacin (in
patients on theophylline) - Outpatient general anesthesia
15
COPD Oral Manifestations
- Halitosis
- Extrinsic tooth stains
- Nicotine stomatitis
- Periodontal disease
- Oral cancer
16
Lung Disease
- Chronic obstructive pulmonary disease (COPD)
- Asthma
17
Asthma Definition
- Chronic inflammatory respiratory disease
- Airway hyperresponsiveness
- Recurrent dyspnea, coughing, wheezing
- Stimuli allergens, URI, exercise, cold air,
medications, chemicals, smoke, anxiety
18
Airway Inflammation and Clinical Symptoms
Inflammation
19
Precipitating or Aggravating Factors
20
Asthma Signs and Symptoms
- Predominant symptoms
- Cough
- Breathlessness
- Wheezing
- chest tightness
- Flushing
- Increased heart rate and prolonged expiration
- May be self-limiting, but severe episodes may
require medical assistance
21
Severity Control
22
Classifying Asthma Severity (age 12)
23
Asthma Classification
- Mild symptoms last less than an hour and do not
occur daily - Moderate Daily symptoms affecting sleep and
activity level - Severe Ongoing symptoms that limit normal
activity and result in emergency hospitalizations
24
Asthma Lab Tests
- No one diagnostic test
- Chest xray, skin testing, sputum smears and blood
counts (for eosinophilia), arterial blood gases - Spirometry (peak expiratory flow meter) before
and after bronchodilator
25
Stepwise Therapy for Asthmafor people 12 years
of age and above
Persistent Asthma
Therapy Preferred Alternative
Step 6 High Dose ICS LABA OCS AND Consider
omalizumab for patients with allergies
Step 5 High Dose ICS LABA AND Consider
omalizumab for patients with allergies
26
Asthma Medical Management
- Plan for avoiding triggers
- Inhaled drugs
- Corticosteroids
- Leukotriene inhibitors
- Beta-adrenergic agonists
- Anticholinergics
27
Asthma Dental Management
Things to do
- Schedule late-morning appointments
- Use rescue inhaler before procedures
- Use pulse oximeter during procedures
- Provide stress-free environment
- good rapport and openness
- may use N2O or oral benzodiazepine
28
Asthma Dental Management
Things to avoid
- Precipitating factors
- Barbiturates and narcotics
- Aspirin, NSAIDs
- Antihistamines (or use cautiously)
- Macrolide antibiotics and ciprofloxacin (in
patients on theophylline)
29
Asthma Managing an attack
- Warning signs
- Frequent cough
- Inability to finish sentence in one breath
- Bronchodilator ineffective
- Tachypnea
- Tachycardia (gt110)
- Diaphoresis
- What to do
- Use short-acting beta-adrenergic agonist inhaler
- Positive-flow oxygenation
- If severe subcutaneous epinephrine, call EMS
30
Asthma Oral Complications
- Mouth breathing complications
- Increased gingivitis and caries secondary to beta
agonist inhaler use - Oral candidiasis secondary to steroid inhaler use
31
Lung Disease
- Chronic obstructive pulmonary disease (COPD)
- Asthma
- Tuberculosis
32
TB Definition
- Pulmonary and systemic disease
- Most common cause M. tuberculosis
- Spread by respiratory droplet
33
TB Signs and symptoms
- Most patients with 1 infection no symptoms
- Cough (scanty, mucoid sputum later purulent)
- Systemic symptoms malaise, unexplained weight
loss, night sweats, fever - Extrapulmonary manifestations lymphadenopathy,
back pain, GI or renal disturbances, heart
failure, neurologic deficits
34
TB Lab Tests
- Positive tuberculin (Mantoux) skin test (does not
mean infection is clinically active) - Xray findings
- progressive primary TB patchy infiltrates,
cavitation, hilar lymphadenopathy - healed primary TB calcified peripheral nodule,
calcified lymph node (Ghon complex) - Sputum smear positive for acid fast organisms
- Confirm with culture and/or molecular tests
35
TB chest xray
36
TB Medical Management
- Drugs chosen based on health of patient,
likelihood of resistant strain - Patients become non-infectious in 3-6 months
- Prophylactic drug treatment for certain close
contacts (young, HIV infected, diabetic)
37
TB Dental Management
- New, active TB treat only urgently and in a
hospital isolation room - After 2-3 weeks of treatment treat normally
- History of TB treat normally if no active
disease - Positive TB test treat normally if no active
disease - Clinical signs suggestive of TB do not treat
38
TB Oral Complications
- Painful, deep tongue ulcers (infrequent)
- Cervical, submandibular lymphadenitis (scrofula)
39
Lung Disease
- Chronic obstructive pulmonary disease (COPD)
- Asthma
- Tuberculosis