Thrombosis - PowerPoint PPT Presentation
1 / 34
Title:
Thrombosis
Description:
... antithrombin III (inactivates thrombin, IXa & Xa) protein C or protein S ... or hyper-estrogenic states (pregnancy) create hypercoagulability by ... – PowerPoint PPT presentation
Number of Views:158
Avg rating:3.0/5.0
Title: Thrombosis
1
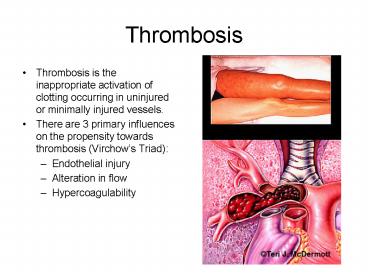
Thrombosis
- Thrombosis is the inappropriate activation of
clotting occurring in uninjured or minimally
injured vessels. - There are 3 primary influences on the propensity
towards thrombosis (Virchows Triad) - Endothelial injury
- Alteration in flow
- Hypercoagulability
2
Fig 4-13 p 131
3
Endothelial injury
- This is the dominant influence on initiation of
coagulation, endothelial injury alone elicits
coagulation (appropriately so!). - The endothelium need not be physically disrupted
to incite thrombosis, anything that perturbs the
delicate balance of coagulate/dont coagulate
maintained by the endothelium can elicit
coagulation. - Injury may be caused by hemodynamic stresses
associated with non-laminar flow due to
dis-kinetic cardiac segments, atherosclerotic
plaques, etc., abnormal endogenous substances
(homocysteine, cholesterol) exogenous substances
(tobacco related substances). - Thrombosis results from exposed ECM and tissue
factor, platelet adhesion, depletion of
anti-coagulant factors.
- Fig 4-7 p 126
4
Alteration of Flow
- Normal blood flow is laminar with cellular
elements located centrally in the vessel lumen
separated from the endothelial wall by a plasma
clear zone. Stasis and turbulent flow disrupt
laminar flow with a number of consequences - platelets contact endothelium
- dilution of activated clotting factors is
prevents - inflow of clot inhibitors is prevented
- Promotion of endothelial activation.
- Stasis elicits thrombosis in the venous system,
cardiac chambers and aneurysmal dilatations. - Plaques disrupt laminar flow in addition to
producing endothelial injury. - Anything that promotes blood viscosity
(hyperviscosity syndromes) promotes stasis
(polycythemia, sickle cell, dehydration, etc.).
5
(No Transcript)
6
Hypercoagulability
- An alteration of coagulation that predisposes to
thrombosis, this is the least frequent cause for
thrombosis but allows the simplest opportunity
for intervention. - Heritable Hypercoagulability states
- Tend to present initially in adolescents or young
women (stroke in the young). - Characterized by recurrent venous thrombosis and
thromboembolism - Lack of Antithrombotic function
- Genetic deficiency in antithrombin III
(inactivates thrombin, IXa Xa) protein C or
protein S mutations (normally promote the
proteolysis of Va VIIIa) that predispose to
venous thrombosis, although infrequent these
conditions in concert with acquired states create
a markedly increased risk of thrombosis. - Extra Prothrombotic function
- Va resistance A factor V mutation (Leiden
mutation) 2-15 of Caucasians, alters to cleavage
site for inactivation of Va by Protein C - Prothrombin 20210A mutation A point mutation in
a non-coding region of the prothrombin gene
resulting in increased levels of prothrombin and
venous thrombosis - Methylene tetrahydrofolate reductase mutation
(MTHFR C677T) A moderate increase in homocyteine
associated with increased arterial venous
thrombosis. This can be mitigated by folate, B6
B12 supplementation. Associated with an
increased risk of neural tube defects
neoplasms. - Constitutively increased factor VIII, IX, XI
fibrinogen levels
7
Hypercoagulable states
Table 4-2 p 132
8
Hypercoagulability
- Acquired Hypercoagulability
- Oral contraceptives or hyper-estrogenic states
(pregnancy) create hypercoagulability by
increasing the synthesis of coagulation factors
and deceased production of antithrombin III. - Certain malignancies and disseminated cancers
release procoagulant tumor products. - Advanced age is associated with increased
platelet aggregation. - Smoking
- Heparin-induced thrombocytopenia syndrome, 5 of
the population, most common with unfractionated
heparin. An antibody forms to heparin-platelet
factor 4 complex resulting in thrombocytopenia
(platelet destruction) and thrombosis through
endothelial activation. - Antiphospholipid antibody syndrome these
individuals have antibodies that can activate
platelets or block protein C activity leading to
hypercoagulability. Usually discovered due to a
slightly elevated PTT (? hypocoagulable, antibody
interferes with intrinsic pathway (lab
phenomena)). Associated with recurrent arterial
venous thromboembolism - Autoimmune disorders may be associated with
hypercoagulability via a similar antiphospholipid
antibody (lupus anticoagulant? slightly elevated
PTT but they are hypercoagulable).
9
Hypercoagulable states
- Table 4-2 p 132
10
Combination Hyper- Hypocoagulable
- Disseminated Intravascular Coagulation (DIC)
- Diffuse endothelial injury results in systemic
activation of the coagulation cascade/thrombosis.
Resulting in - Microthrombi (occasionally macrothrombi) which
impair tissue perfusion CNS, heart, renal, lungs
are particularly at risk. - Depletion of coagulation factors and production
of fibrinolytic agents that result in systemic
hemorrhage. - What do you do?
11
Morphology of Thrombi
- Thrombi may form any where in the vascular
system, they vary in size and shape depending on
their site of origin and how firmly they are
attached at their origin. - Arterial thrombi
- Found in areas of active flow
- Commonly show layering of platelets fibrin
(Lines of Zahn) - Cardiac aortic thrombi tend to be non-occlusive
(???flow). - Cardiac mural thrombi based on akinetic/dyskinteic
wall segments - Tend to propagate distally often with
embolization (can propagate retrograde) - Atherosclerotic plaques, endothelial injury,
areas of turbulent flow serve as nidus - Valvular irregularities may be emboli source
12
Fig 4-14 p132
13
Venous thrombosis
- Characteristically in areas of low/no flow or
turbulent flow. - Superficial thrombi usually occur in enlarged
saphenous veins. - Deep vein thrombi (DVT) generally occur in veins
proximal to the knee and due to the abundant
collateral venous system are asymptomatic in 50
of instances prior to an embolic event. The
situations associated with increased risk of DVT
are legion, anything that involves prolonged
immobilization (? gt 8 hours, particularly
associated with dehydration) CHF, trauma
(including surgical), pregnancy and post-partum
states and malignancy. - Often associated with inflammatory changes (
thrombophlebitis).
14
The Fate of the Thrombus
- Once formed the thrombus has a limited number of
fates - Propagation with subsequent vessel occlusion,
depending on the location and type of vessels the
sequelae may be minor (superficial vein
thrombosis) or catastrophic (stroke, MI, etc.). - Embolization to downstream sites (PE)
- Dissolution by fibrinolytic activity (a
therapeutic intervention) - Organization recanalization, endothelial cells,
smooth muscle cells and fibroblasts create
vascular channels in the thombus.
15
Fig 4-15 p 134
16
Fig 4-16 p 135
17
Organized pulmonary embolus
18
Clinical Significance
- Thrombi are important because they
- Cause obstruction of arteries and veins (arterial
obstruction worse) - Are possible sources of emboli (worse in venous
obstruction)
19
Embolism
- Embolism refers to any intravascular mass carried
by blood flow to a site distant from its origin,
most arise from thrombi other emboli may consist
of fat, gas bubbles, atherosclerotic debris,
tumor fragments, bone marrow, foreign bodies,
particulate matter, etc. Emboli lodge in vessels
too small to permit further passage, the
distribution depending on blood flow drown-stream
from the source.
20
Pulmonary Thromboembolism
- PE has a reported incidence of 20-25/100,000
hospitalized patients, gt95 of PEs originate from
DVTs. Increased risk with immobilization,
post-op and CHF (venous stasis). - Most PEs (60-80) are clinically silent.
- Obstruction of medium sized pulmonary arteries
may cause pulmonary hemorrhage but pulmonary
infarction is rare due to the bronchial blood
supply. - Obstructon of 60 of the pulmonary circulation
results in right-heart failure, cardiovascular
collapse or sudden death. (Saddle embolus). - Multiple emboli over time may result in pulmonary
hypertension.
21
Fig 4-19 p 138
22
(No Transcript)
23
- Fig 4-17 p 136
24
Systemic Thromboembolism
- Systemic emboli most often arise from
intracardiac mural thrombi, often associated with
MI. 25 arise from dilated LA due to valvular
disease. - Atherosclerotic plaques are frequently the source
of non-cardiac emboli. - The consequences of arterial occlusion depends
on collateral circulation and tissue sensitivity
to hypoxia.
25
- Common sites of arrest
- ICA branches, especially the MCA
- Mesenteric artery branches
- Renal artery branches (however 75 loss of renal
function before symptomatic) - Paradoxical emboli
- Intracardiac (R?L) shunt (patent foramen ovale or
ASD) of emboli can occur particularly with
equalization of pressures (? right side with
pulmonary hypertension, ? left side CHF, MI,
etc.).
26
Fat Embolism
- Fat embolism results form the release of
microscopic fat globules after long bone
fracture, fat embolism occurs in 90 of severe
skeletal trauma but 10 have any clinical signs.
- 10 of cases are fatal and present as acute
pulmonary failure 1-3 days post injury. - Thrombocytopenia, petechial rash and CNS
deterioration are frequently seen in severe
cases. - Fat emboli produce symptoms due to vessel
occlusion but also activate platelets and WBCs,
fatty acid release causes direct endothelial
injury.
27
Fat emboli marrow elements with fat in a vessel
lumen
28
Air Embolism
- Gas bubbles in the vasculature can cause
obstruction resulting in ischemia, room air may
enter the circulation any time large low pressure
venous structures are disrupted (thoracic,
pelvic, obstetric, lower extremity, neck and
spine procedures), approximately 100 mls of air
is required to be symptomatic. - Decompression sickness
29
Amniotic fluid embolism
- A rare (1/50,000 deliveries) but catastrophic
(gt80 mortality) complication of labor, due to
infusion of amniotic fliud into the maternal
circulation. The presentation is of acute severe
dyspnea, cyanosis, DIC, hypotension, shock,
seizures and coma.
Amniotic fluid embolus, fetal squamous epithelial
cells in a pulmonary arteriole
30
30 year old male presented 30 minutes after
being accidently shot with a pneumatic nail gun.
BP 86/60, HR 133. After 20 minutes he
complained of severe left leg pain
Femoral
Profunda
31
Conclusions
- Thrombosis is the inappropriate activation of
hemostasis - Vircows triad describes the predisposing factors
for thrombosis - Endothelial injury/activation
- Alteration in flow
- Hypercoaguability
- Normal endothelial function is a delicate balance
between pro- and anti-thrombotic influences,
normally anti-thrombosis predominates. - Abnormal flow results in
- Stasis
- Loss of dilution of activated factors
- Loss of the influx of clot inhibitors
- Promoting endothelial activation
- Atherosclerotic plaques elicit
- Abnormal flow patterns
- Direct endothelial injury
32
Conclusions
- 6. Hypercoagulability
- Inherited
- Acquired
- 7. Hyperestrogenic states, malignancy, age,
smoking, heparin induced, thrombocytopenia, MI,
A-fib, prosthetic valves, etc. - 8. Thrombi may propagate, embolize, dissolve,
organize and recanalize. - 9. Venous thromboembolism
- DVT-50 are asymptomatic prior to an embolic
event - 10. Arterial thrombosis
- Often results in obstruction with ischemia unless
a collateral circulatory system is readily
available - Embolization to distal vasculature
- 12. DIC causes widespread microthrombi but
presents as a bleeding diathesis due to systemic
activation of the fibrinolytic system
33
Conclusions
- 13.Anything reaching the intravascular system can
embolize - Fat
- Air
- Amniotic fluid
- 14. PE
- 1/2 -3/4ths are silent
- Can cause acute right heart failure and death
- 15. Fat embolism is common (90) is severe
skeletal trauma, usually is asymptomatic but can
present as acute pulmonary failure,
thrombocytopenia and CNS deterioation 1-3 days
post trauma.
34
(No Transcript)