Intranasal Medications in clinical practice - PowerPoint PPT Presentation
1 / 28
Title:
Intranasal Medications in clinical practice
Description:
Molecules absorbed through the gut, including all oral medications enter the ' ... Nasally delivered medications avoid the gut so do not suffer first pass ... – PowerPoint PPT presentation
Number of Views:137
Avg rating:3.0/5.0
Title: Intranasal Medications in clinical practice
1
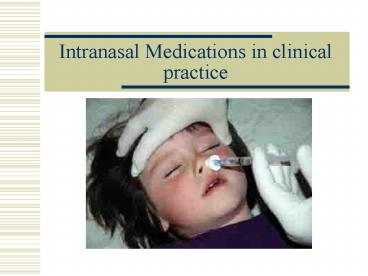
Intranasal Medications in clinical practice
2
Transmucosal medication delivery
- Is this really a novel idea?
- Commercially available transmucosal drugs
- Actiq oral (transmucosal fentanyl lollipop)
- Nitroglycerin Sublingual.
- Stadol (butorphanol) - Intranasal opiate.
- Fentora - Transmucosal fentanyl tablet
- DDAVP - Intranasal delivery route.
- Migraine medications Migranol (DHE), etc.
- Influenza Vaccine - Intranasal system is
available. - Active area of pharmacology research
3
Transmucosal Drug Delivery
- Many IV medications, including analgesics and
sedatives, can be delivered transmucosally,
though not currently available for that
indication commercially - Large literature base to support their use.
- Generic drugs are available, cutting costs
significantly.
4
Why Intranasal (IN) medications?
- This delivery route has several advantages
- Its easy and convenient
- Almost everyone has a nose
- The nose is a very easy access point for
medication delivery - even easier to access than
IM or IV sites, much easier than rectal delivery - No special training is required to deliver the
medication - No shots are needed
- Painless
- Low risk
- It eliminates any risk of a needle stick to the
medical provider
5
Intranasal Medication Administration
- Needleless Intranasal Medication administration
offers a truly Needleless solution to drug
delivery. - Superior Intranasal medication administration
generally results in superior drug delivery to
the blood stream compared to other transmucosal
routes. - The remainder of this discussion will surround
the topic of intranasal drug delivery issues.
6
Lecture Outline
- Part 1
- Discuss the concept of Off-label medication
- General principles of intranasal medication
delivery - Part 2 Intranasal medications in clinical
practice - EMS
- Emergency Medicine
- Anesthesia
- Hospice
7
IN medications Off-label use
- What is off-label use
- Drugs are approved for specific indications in
specific subpopulations by specific route of
delivery - All other uses are off label
- Common Examples of off-label use
- IV lorazepam for status epilepsy in children
- Most IV drugs given to children (80), pregnant
women - Most antidotes for drug overdoses
- ACLS drugs down an endotracheal tube
- H2 blockers for allergies
8
IN medications Off-label use
- Why are so many common uses off-label
- It costs about 650 million to bring a drug to
market for an indication - Once it is on the market, clinicians can use it
as they choose for any indication. - Unless there is a HUGE financial incentive to
seek another indication, the pharma company will
not spend the money to get another indication
9
IN medications Off-label use
- Is it OK to use drugs off-label
- Yes in fact is is expected this will occur and
this actually helps advance medical care - U.S Supreme court on off-label use off-label
usage of medical devices is an accepted and
necessary corollary of the FDAs mission health
care practitioners can prescribe or administer
any legally marketed device to a patient without
limitation or interference.
10
IN medications Off-label use
- Center for drug evaluation and research on
off-label use Any approved product may be used
by a licensed practitioner for uses other than
those stated in the product label. - FDA on off-label use Off-label use is a
well-established principle that has allowed
doctors to discover new and beneficial uses for
previously approved drugs.
11
IN medications Off-label use
- Nice summary on the topic from and Australian
committee - Routine off-label use (or on-label use) can be
justified if there is high-quality evidence
supporting efficacy or effectiveness, and
sufficient evidence about the medicines safety
profile to suggest and overall reasonable benefit
risk for a given clinical context - Conclusion
- Off-label use is acceptable.
- Most intranasal drugs are off-label but that is
OK if they provide justifiable benefits.
12
Understanding IN delivery General principles
- First pass metabolism
- Nose brain pathway
- Lipophilicity
- Bioavailability
13
First pass metabolism
- Molecules absorbed through the gut, including all
oral medications enter the portal circulation
and are transported to the liver. - Liver enzymes then break down most of these drug
molecules and only a small fraction enter the
bodys circulation as active drug. - This process is called First Pass Metabolism.
- POINT Nasally delivered medications avoid the
gut so do not suffer first pass metabolism.
14
First pass metabolism
15
Nose brain pathway
- The olfactory mucosa (smelling area in nose) is
in direct contact with the brain and CSF. - Medications absorbed across the olfactory mucosa
directly enter the CSF. - This area is termed the nose brain pathway and
offers a rapid, direct route for drug delivery to
the brain.
Olfactory mucosa, nerve
Brain CSF
Highly vascular nasal mucosa
16
Lipophilicity
Non-lipophilic molecules
- Lipid Loving
- Cellular membranes are composed of layers of
lipid material. - Drugs that are lipophilic are easily and rapidly
absorbed across the mucous membranes.
Lipophilic molecules
Cell Membrane
Blood stream
17
Bioavailability
- How much of the administered medication actually
ends up in the blood stream. - Examples
- IV medications are 100 bioavailable.
- Most oral medications are about 5-10
bioavailable due to destruction in the gut and
liver. - Nasal medications vary, but when the right drug
is delivered in the right way can approach 80.
18
Bioavailability
- Graph demonstrating naloxone serum concentrations
when given via IV and IN routes. - Note that IV and IN serum levels are similar
after about 5 minutes.
19
Intranasal Medication Administration
Bioavailability
- Not all drugs can be delivered via the nasal
mucosa. - Factors affecting bioavailability
- Medication characteristics.
- Medication volume and concentration.
- Nasal mucosal characteristics.
- Delivery system characteristics.
- Mucosal surface area coverage.
- Medication particle size.
20
Intranasal Medication Administration Factors
Affecting Bioavailability
- Medication Characteristics
- Drug characteristics that affect bioavailability
via the nasal mucosa include - Molecular size.
- Lipophilicity.
- pH.
- Drug concentration.
- Properties of the solution the drug is
solubilized within.
21
Intranasal Medication Administration Factors
Affecting Bioavailability
- Volume and concentration
- Low volume - High concentration.
- Too large a volume or too weak a concentration
may lead to failure because the drug cannot be
absorbed in high enough quantity to be effective. - Ideal volume for nasal delivery is 1/4 to 1/2 ml
per nostril - Volumes over 1 ml per nostril are too large and
may result in runoff out of the nostril.
22
Intranasal Medication Administration Factors
Affecting Bioavailability
- Nasal mucosal characteristics
- If there is something wrong with the nasal mucosa
it may not absorb medications effectively. - Examples
- Vasoconstrictors such as Afrin, cocaine prevent
absorption. - Bloody nose, nasal congestion, mucous discharge
all prevent mucosal contact of drug. - This might be overcome with suction prior to drug
delivery - Destruction of nasal mucosa from surgery or past
cocaine abuse no mucosa to absorb the drug.
23
Intranasal Medication Administration Factors
Affecting Bioavailability
- Delivery system characteristics
- Nasal mucosal surface area coverage
- Larger surface area delivery higher
bioavailability. - Particle size
- Particle size 10-100 microns adheres best to the
nasal mucosa. - Smaller particles pass on to the lungs, larger
particles form drop and rapidly run-out of the
nose.
24
Bioavailability and Particle size
- Compared to drops, atomized medication results
in - Larger surface area of coverage.
- Smaller liquid particle size allowing thin layer
to cover mucosa. - Less run-off out the nasal cavity.
25
Intranasal Medication Administration Summary
- Points
- Nasal drug delivery is convenient and easy, but
it may not always be effective. - Nasal drug delivery cannot completely replace the
need for injections. - Being aware of the limitations and using the
correct equipment and drug concentrations will
assist you in predicting times when nasal drug
delivery may not be effective.
26
IN drug delivery Requirements
- Appropriate Drug
- Known to be bioavailable across the nasal mucosa
- Appropriate Concentration
- Most concentrated form available
- Appropriate patient
- Requires treatment
- Nasal mucosa healthy, free of obvious severe
bleeding, thick mucous, etc
27
IN drug delivery Conclusions
- IN drug delivery is
- Convenient, easy and effective for selected
situations - May result in reduced needlestick risk
- Can improve and simplify your practice and your
patients experience - Will NOT replace the need for injections
28
Nasal Drug Delivery What Medications?
- There are numerous peer reviewed articles on this
topic is you search PubMed or other internet
sites for specific indications using key words
such as intranasal and the medication or
application you desire.