Hypersensitivity Reactions - PowerPoint PPT Presentation
1 / 17
Title:
Hypersensitivity Reactions
Description:
Urticaria (hives, wheal & flare response) Clinical Manifestations of Type I ... If the patient is allergic a wheal & flare response occurs ... – PowerPoint PPT presentation
Number of Views:220
Avg rating:3.0/5.0
Title: Hypersensitivity Reactions
1
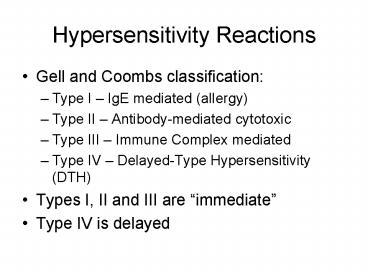
Hypersensitivity Reactions
- Gell and Coombs classification
- Type I IgE mediated (allergy)
- Type II Antibody-mediated cytotoxic
- Type III Immune Complex mediated
- Type IV Delayed-Type Hypersensitivity (DTH)
- Types I, II and III are immediate
- Type IV is delayed
2
Type I Hypersensitivity
- Antigens are called allergens
- Unknown why people get allergies, but there is a
strong genetic predisposition (called atopy) - Hallmark is inappropriate production of IgE
against allergens that cause mast cell
degranulation (see fig 15-2) - Normally IgE/mast cell activity should be
directed against parasitic infections
3
Type I Hypersensitivity
- Mediators of Type I hypersensitivites
- Mast cell granule contents (early effects)
- Histamine and Heparin - ? vascular permeability,
smooth muscle contraction (intestines, bronchi),
mucus secretion - Chemotactic factors attract eosinophils and
neutrophils - Proteases mucus secretion, complement
activation, degradation of blood vessel basement
membrane - Later Effects
- Leukotrienes and prostaglandins secreted after
tissue disruption caused by mast cell
degranulation, effects are similar to histamine - Arrival of proinflammatory eosinophils and
neutrophils
4
(No Transcript)
5
Clinical Manifestations of Type I
- Systemic anaphylaxis
- Allergen gets into the blood stream
- Dyspnea, ?BP, bronchole constriction, GI and
bladder smooth muscle contration, shock, death
within minutes if untreated - Treatment - epinephrine
- Allergic rhinitis (hay fever)
- Inhaled allergen triggers reaction in nasal
mucosa - Watery exudate from nose, eyes, upper respiratory
tract, sneeezing and coughing
6
Clinical Manifestations of Type I
- Asthma
- Allergic asthma due to inhaled airborne
allergens (pollens, dust, fumes, etc) - Intrinsic asthma triggered by cold, exercise
- Reaction develops in lower respiratory tract
- Bronchoconstriction, airway edema, mucus
secretion, inflammation - Food allergies
- Ingestion of allergen
- Vomiting and diarrhea
- If allergens are absorbed into bloodstream,
reactions can occur where allergen deposits - asthma-like symptoms
- Urticaria (hives, wheal flare response)
7
Clinical Manifestations of Type I
- Atopic Dermatitis (allergic eczema)
- Often occurs in young children
- Red skin rash
- Strong hereditary predisposition
8
Type I Hypersensitivity
- Skin testing
- Potential allergens are injected or scratched
into the skin - If the patient is allergic a wheal flare
response occurs - RIST radioimmunosorbent test similar to RIA,
non-invasive way to identify allergies
9
Type I Hypersensitivity
- Treatment
- Avoid allergen if possible
- Antihistamines, or anti-prostaglandins
- Hyposensitization injections of low doses of
allergen may cause a shift from IgE to IgG as the
dominant antibody formed.
10
Type II Hypersensitivity
- Antibody-mediated Cytotoxic HS
- Antibodies (IgM or IgG) bind to cell surface
antigens. Antigen/antibody complex may lead to - Complement activation ? lysis
- ADCC
- Opsonization ? phagocytosis
- These are normal reactions, but when they cause
unwarranted tissue damage, they are considered a
hypersensitivity.
11
Type II Hypersensitivity
- Examples of Type II HS
- Transfusion reactions
- To ABO blood groups
- To other RBC blood groups
- Hemolytic disease of the newborn
(erythroblastosis fetalis) - Drug-induced hemolytic anemia (penicillin)
12
Type III Hypersensitivity
- Immune Complex Disease
- Antibody (IgG) / attaching to soluble antigen
leads to complex formation - Immune complexes may deposit in
- Blood vessel walls (vasculitis)
- Synovial joints (arthritis)
- Glomerular basement membrane (glomerulonephritis)
- Choroid plexus
13
Type III Hypersensitivity
- Damage occurs due to
- Anaphylatoxin release due to complement
activation (C3a, C5a) which then attracts
neutrophils, and causes mast cell degranulation - Neutrophils have trouble phagocytosing stuck
immune complexes so they release their granule
contents leading to more inflammation - Platelet aggregation also results from complement
activation - These effects are also known as the Arthus
reaction
14
Type III Hypersensitivity
- Localized reactions
- edema and redness (erythema) and tissue necrosis
of the affected tissue - Can occur in the skin following insect bites
- Can occur in the lungs
- E.g. farmers lung from inhaling particles from
moldy hay
15
Type III Hypersenstivity
- Generalized reactions
- Serum sickness (following treatment with
antiserum to a toxin) - Autoimmune diseases
- SLE
- Rheumatoid arthritis
- Drug reactions (penicillin)
- Infectious diseases
- Meningitis, hepatitis, malaria, mono etc.
16
Type IV Hypersensitivity
- Delayed type hypersensitivity (DTH)
- TH cells that have been sensitized by an
antigen develop a TH1 and (sometimes a TC
response) leading to macrophage recruitment and
activation. - First noticed with reaction to tuberculosis
bacteria (tuberculin reaction) - Hallmarks of type IV is the large number of
macrophages at the reaction site, and that it
takes an average of 24 hrs to manifest after
repeat exposure.
17
(No Transcript)