Malaria statistics for under 5, including morbidity - PowerPoint PPT Presentation
1 / 11
Title:
Malaria statistics for under 5, including morbidity
Description:
If countries can get well organized & supervised systems lots of useful data could be collected ... logistics big problem , plane mostly- drugs usually given ... – PowerPoint PPT presentation
Number of Views:35
Avg rating:3.0/5.0
Title: Malaria statistics for under 5, including morbidity
1
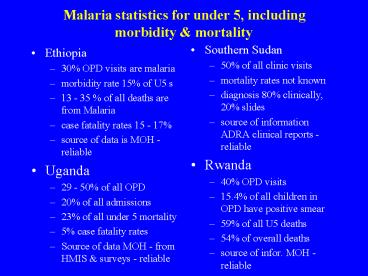
Malaria statistics for under 5, including
morbidity mortality
- Southern Sudan
- 50 of all clinic visits
- mortality rates not known
- diagnosis 80 clinically, 20 slides
- source of information ADRA clinical reports -
reliable - Rwanda
- 40 OPD visits
- 15.4 of all children in OPD have positive smear
- 59 of all U5 deaths
- 54 of overall deaths
- source of infor. MOH - reliable
- Ethiopia
- 30 OPD visits are malaria
- morbidity rate 15 of U5 s
- 13 - 35 of all deaths are from Malaria
- case fatality rates 15 - 17
- source of data is MOH - reliable
- Uganda
- 29 - 50 of all OPD
- 20 of all admissions
- 23 of all under 5 mortality
- 5 case fatality rates
- Source of data MOH - from HMIS surveys -
reliable
2
Malaria statistics for under 5, including
morbidity mortality
- Somalia
- the health facilities are supported by UNICEF and
data is analysed by UNICEF
- Tanzania
- 31 of all OPD cases
- 15 of admissions
- 20 of U5 mortality
- Source of data MOH - reliable
3
Comments on the data / statistics
- Different countries are collecting on different
indicators - although some are different - Sudan figures are only for a limited population
that can be accessed - Case fatality rates give an indication of quality
of the services but may also depend on endemicity
of the areas e.g. hypoendemic areas are epidemic
prone and have higher fatality - Several factors affect the reliability of the
data including - diagnostic facilities - most diagnosis in the
region is clinical - system for recording and compiling of data-
systems may be in place but are sometimes not
utilised properly - motivation, work load and experience of the
person(s) collecting the data - the small proportion of patients that are treated
in the facilities from which the data is
collected (many cases are treated outside the
formal health sector) . - If countries can get well organized supervised
systems lots of useful data could be collected
4
Protocol for malaria case finding management
- Somalia
- No national protocol. There are UNICEF, WHO
guidelines developed through the working groups.
The availability utilisation of the guidelines
depends on the agency. (Somaliland does have
protocol. - Rwanda
- There is a national protocol - recently revised -
implementation at service delivery level varies
by region, the supervision system the persons.
Policy does not allow community level
distribution. - Uganda
- there is a national protocol - training has been
done but implementation is dependent on the area,
work ethics, access to drugs, supervision.
Community component designed - but not yet in
community
5
Protocols cont.
- Tanzania
- Has the protocol including the national drug
policy, service providers have been trained at
all levels and the guidelines are available.
They are used, there is close supervision by the
DHMT - Southern Sudan
- standard treatment guidelines developed for first
level workers, primary health care workers
hospital level used by the 42 NGOs under UNOLS - Ethiopia
- Protocol developed, disseminated to all levels
but implementation depends on level of
supervision
6
Drug policies for uncomplicated malaria for
severe malaria - availability of drugs
- Tanzania
- first line drug for uncomplicated malaria is SP
(since August 2001) available at all levels,
including community level - second line drug is Amodiaquine available in the
health facilities - Drugs supplied by the national medical stores
through essential drug kit to government health
units - sometimes there is drug shortages. There
are also other sources of drugs e.g. private
pharmacies - limitations to access by communities include cost
(cost about 1 for a course of treatment),
logistics for distribution of drugs education
of the community - Quinine recommended for severe malaria available
mostly at hospital level though recommended for
levels down to dispensary level (level 2)
7
Drug policies and availability cont...
- Rwanda
- first line is combination of SP AQ not yet in
use all through the country - in some parts
chloroquine is till being used. - Supplies are there but the drugs are expensive
2-3 for a course . Fear of poor quality service
is another limiting factor. - Work with the private drug shops, ordinary shops
and community level not yet allowed - Quinine is drug for severe malaria at all levels
- Ethiopia
- has drug policy. SP is first line for
uncomplicated malaria- drugs are affordable -
sometimes unavailable in health facilities but
available with private vendors though more
expensive(less than 0.5) - Quinine used for severe malaria - in hospitals
higher level health units - ordinary shops do not sell antimalarials - it is
drug shops pharmacies that sell drugs - Community health workers where they exist - carry
the antimalarial drugs - depends on different
regions of the country - community education going on -
8
Drug policies availability
- Southern Sudan
- first line is CQ available to lowest level run by
CHW. In health centres there is CQ SP. Severe
cases Quinine IV if qualified staff - otherwise
oral quinine - drugs only available from NGO or from
neighbouring country - poor access to health facilities referrals
- logistics big problem , plane mostly- drugs
usually given free - cost sharing is being
started in SPLM area - Uganda
- National drug policy still has to undergo some
approvals to be used at community level -
combination of SP/CQ - most people still using
chloroquine. Community education going on. - Limitations include policy bureaucracies
community education - Quinine for severe malaria - at all levels
9
Drug Policies cont.
- Somalia
- drug policies not there but since June RBM
started - protocol from UNICEF WHO being used
that recommends SP - still just being introduced
to the health workers. In most of the areas
there are lots of drugs sellers not under any
control - first line is Chloroquine- usually
taken only what can be afforded - usually
incomplete dose. In the world vision areas,
Chloroquine is used as first line, second line SP
- quinine available for severe malaria if there
is a qualified staff. Logistics a big problem
10
Summary of obstacles to accessibility to drugs.
- Logistics
- Availability
- affordability
- security
- new programs
- bureaucracies
- lack of qualified staff
- poor quality of services
- lack of information on correct drugs, sources of
drugs, dosages etc
11
What can NGOs do to enable community members
access treatment for malaria?
- Empower communities with knowledge - use all
available channels for sharing information - NGOs have ability to do community level demand
creating services - can work with communities to
demand services and come with solutions - however
creation of demand should go on with making the
services available e.g. from Africare - Uganda
which created demand then linked with government
to make the services available e.g. of
innovative story from Southern Sudan - addressing factors that affect availability of
drugs - - need to bring together key players to assess the
malaria situation and come up with joint
solutions correct mix of interventions - NGOs working closely with both government
communities to generate solutions - linkage between health component income
generating sectors