201 Immunology: goals - PowerPoint PPT Presentation
1 / 53
Title:
201 Immunology: goals
Description:
Ligation of the T cell's receptor for antigen results in an initial activation ... ligation of CD28 by B7. on the APC. Ligation of the TCR without co ... – PowerPoint PPT presentation
Number of Views:34
Avg rating:3.0/5.0
Title: 201 Immunology: goals
1
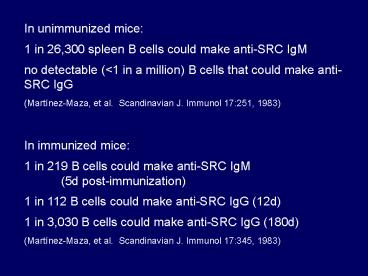
In unimmunized mice 1 in 26,300 spleen B cells
could make anti-SRC IgM no detectable (lt1 in a
million) B cells that could make anti-SRC
IgG (Martínez-Maza, et al. Scandinavian J.
Immunol 17251, 1983) In immunized mice 1 in
219 B cells could make anti-SRC IgM (5d
post-immunization) 1 in 112 B cells could make
anti-SRC IgG (12d) 1 in 3,030 B cells could make
anti-SRC IgG (180d) (Martínez-Maza, et al.
Scandinavian J. Immunol 17345, 1983)
2
(No Transcript)
3
(No Transcript)
4
T CELL DEVELOPMENT AND ACTIVATION
- There are a lot of similarities between T and B
cells, in their development - arise from hematopoietic precursors that are
generated in the bone marrow - undergo similar DNA rearrangements to generate
the genes for their antigen receptor molecules - have the capacity to respond to nearly any
antigen - the initial stages of development are
antigen-independent, with final differentiation
occurring after exposure to antigen - cells that express antigen-receptors that react
with self are eliminated
5
- However, there are some significant differences
- since the T cell receptor can interact with
antigen only when it is presented in association
with self-MHC molecules, T cells need to be able
to bind to a complex of self MHC Ag peptide - in addition to this (perhaps because of this) T
cells do not develop in the bone marrow, they
undergo development in a specialized organ, the
thymus.
6
- T lymphocytes or T cells got their name from
original observations that indicated that they
were thymus-derived lymphocytes. - T cell precursors travel from the bone marrow to
the thymus
7
- Following development into mature,
antigen-responsive T cells, these T cells emerge
from the thymus and migrate to secondary lymphoid
tissues, where they interact with antigen,
antigen-presenting cells, and other lymphocytes
8
- The importance of the thymus in T cell
development is demonstrated by inherited immune
deficiencies people that do not have a thymus
(DiGeorges syndrome, aka Thymic Aplasia) do not
develop functional T cells. - DiGeorges syndrome results from a developmental
defect the failure of the third and fourth
pharyngeal pouches to develop, which results not
just in thymic defects, but also in absent
parathyroids and in aortic arch defects. - Thymectomy early in life reduces the ability to
produce T cells. - Thymectomy later in life does not markedly impair
T cell number. - In fact, the thymus decreases in size with age.
- However, the thymus can still produce new T cells
up to middle-age, especially in situations where
there is loss of T cells (HIV/AIDS).
9
- While in the thymus, immature T cells, or
thymocytes, undergo several changes that allow
them to develop into mature T cells, ready for
contact with antigen. - Thymocytes interact with thymic epithelial cells
and various other cells while in the thymus.
10
- The thymus is composed of several lobes, each of
which has cortical and medullary regions
11
- The cortex contains immature thymocytes in close
contact with thymic epithelial cells. - Medullary areas contain more mature thymocytes,
epithelial cells, and dendritic cells and
macrophages
12
- During thymic differentiation, the great
majority of thymocytes die by apoptosis, and are
ingested by macrophages. - Only a small minority of these T cell progenitors
make it out as mature T cells
13
- Thymic development occurs in two phases
- production of T cell receptors for antigen, by
- rearrangement of the TCR genes
- 2) selection of T cells that can interact
effectively with self-MHC
14
- Changes in the expression of cell-surface
molecules accompany the thymic differentiation of
T cells - entering thymocytes are TCR, CD3, CD4, and
CD8-negative - as thymocytes mature, and undergo rearrangement
of their TCR genes to generate a functional TCR,
they begin to express CD3, CD4, and CD8 - mature T cells ready to go to the periphery are
TCR/CD3, and either CD4 or CD8 positive
15
First phase of thymic development rearrangement
of TCR genes to produce a functional TCR
- Progenitor T cells enter the thymus
(sub-capsular region of the outer cortex). - These cells do not have rearranged TCR genes and
lack expression of characteristic T cell surface
molecules. - Interaction with thymic stromal cells induces
these progenitor T cells to proliferate. - These immature thymocytes do not yet express CD4
or CD8, molecules that are expressed by mature T
cells double-negative thymocytes.
16
- There are two types of T cell receptors gd and
ab - ab TCR T cells are the most abundant, by far
(or g d chain)
17
- Unlike B cells, in which the genes that encode
the BCR rearrange in a set order, the TCR b, g,
and d genes start to rearrange at about the same
time. - If a productive g or d rearrangement occurs
first, the T cell is committed to that lineage,
and stops further rearrangement of the b TCR
gene.
18
However, if b is rearranged first, then the T
cell continues to proliferate, and undergoes
further rearrangements. This results either in
rearranged a TCR gene, yielding an ab TCR lineage
cell, or rearranging g and d genes, resulting in
a gd TCR cell.
19
- Rearrangements that lead to an ab T cell begin
the rearrangement of the b TCR gene. - The first step is D-J joining, followed by VDJ
rearrangement. - Expression of b chain stops further b chain
rearrangements.
20
- b chain is then expressed on the surface of the
thymocyte in association with a surrogate a chain
(pTa). - Following this, there is rearrangement of the a
TCR gene, resulting in a functional a chain, and
in the expression of surface TCR, in association
with other T cell-associated cell surface
molecules.
21
(No Transcript)
22
- During this process, a cell that makes an
unproductive a chain rearrangement can try again
until gets a good a chain, or it exhausts its
possibilities
23
- Thymocytes that have a functional b
rearrangement, and express ab or b the
surrogate a chain (pTa) are induced to express
both CD4 and CD8 simultaneously these are
called double-positive cells. - Immature T cells that do not undergo a productive
rearrangement die by apoptosis.
24
Second phase of thymic development selection
of T cells that can interact with self MHC and
antigen
- This applies only to ab TCR-bearing cells (gt95
of T cells). - gd T cells are not restricted to interactions
with MHC class I or class II molecules - This phase of T cell development consists of two
steps - positive selection (TCR that can interact with
self-MHC) - negative selection (eliminate self-reactive cells
that are stimulated by MHC self)
25
Positive Selection
- Positive selection refers to the selection of
thymocytes that are able to bind to, and interact
with, self-MHC molecules - In positive selection developing thymocytes
continue to live if they bind MHC well enough to
receive a signal through their TCR. - This signal is mediated by the interactions of
these cells with MHC-expressing thymic cortical
epithelial cells. - The 95 of thymocytes that do not receive this
signal undergo apoptosis.
26
Positive selection takes place in the cortex of
the thymus lobules
27
- These CD4 CD8 TCR thymocytes interact with
thymic epithelial cells that express both MHC
class I and MHC class II molecules, complexed
with self-peptides. - Thymocytes that bind MHC survive those that
dont bind to self-MHC die. - TCR a chain rearrangements can continue during
positive selection, allowing cells to explore
alternative a chains for MHC binding. - Once a T cell is positively selected, TCR
rearrangement stops.
28
- The expression of either CD4 or CD8 by a given T
cell is determined during positive selection,
leading to single-positive cells (CD4 or
CD8-positive). - Those cells that have a TCR that binds to MHC
class II end up as CD4 single-positive cells - Those that bind MHC class I as CD8 positive
cells
29
(No Transcript)
30
Negative Selection
- Negative selection refers to the elimination of
those thymocytes that bind to self-MHC molecules
self with high affinity. - In negative selection developing thymocytes die
if they bind MHC self peptides too well
(strongly enough so that they would be activated
by this interaction, via signaling through their
TCR).
31
- Thymocytes undergo negative selection in the
medullary region
32
- There, they interact with antigen-presenting
cells (dendritic cells, macrophages) that express
self-antigens MHC class I or MHC class II
molecules. - Thymocytes that bind to self MHC too strongly
are eliminated as possibly self-reactive cells,
and undergo apoptosis. - If self-reactive T cells were allowed to exit the
thymus, such cells would mediate autoimmune
disease.
33
- Some T cells are reactive with self molecules
that are not expressed in the thymus - such cells can be eliminated in peripheral
lymphoid tissues by the induction of anergy - signal 1 only - incomplete stimulation via their
TCR)
thymocyte
34
- T cells that exit the thymus have undergone a
series of changes that allow them to - develop a functional TCR
- interact with self-MHC
- while eliminating self-reactive T cells
35
The specificity or affinity of positive selection
must differ from that of negative selection
36
(No Transcript)
37
(No Transcript)
38
Antigen-driven T cell Differentiation in
Secondary Lymphoid Organs
- Mature T cells leave the thymus and migrate to
secondary lymphoid tissues (lymph nodes, spleen,
mucosa-associated lymphoid tissue), recirculating
via the blood and lymph, just like mature B cells
do. - Mature T cells are longer lived than mature B
cells, and can survive for years without
antigenic stimulation.
39
- Unlike B cells, which have just one type of
terminally-differentiated cell (plasma cell),
there are various types of effector T cells - CD8 T cells, which can differentiate into
cytotoxic T cells - CD4 T cells, which can become either TH1 or TH2
helper cells.
40
T cells interact with antigen in the T cell-rich
areas of peripheral lymphoid tissues
41
T cells (and B cells) are targeted to, and enter,
secondary lymphoid organs by their expression of
various adhesion molecules. These molecules
interact with ligands expressed on endothelial
cells, allowing these lymphocytes to bind and
enter these lymphoid organs
42
There, they can interact with antigen-presenting
cells (dendritic cells, macrophages, B cells) and
be stimulated on encounter with an appropriate
antigen, and function as helper T cells,
interacting with B cells and other lymphocytes.
43
(No Transcript)
44
(No Transcript)
45
- Ligation of the T cells receptor for antigen
results in an initial activation signal (first
signal), as is true for B cells. - Again, as with B cells, this first signal is not
sufficient to activate the cell - second signals (co-stimulatory signals) are
necessary for activation - The principal co-stimulatory signal for T cells
is delivered via ligation of CD28 by B7 on the
APC
46
- Ligation of the TCR without co-stimulation
results in T cells becoming non-responsive or
apoptotic
47
Activation, proliferation, survival
modified from Laâbi, Y. and A. Strasser.
Science 289883, 2000
48
- T cell signaling occurs via the cytoplasmic tails
of the molecules that make up the CD3 complex,
which is associated with the TCR.
49
- These associate with protein tyrosine kinases and
initiate intracellular signaling that results in
altered gene expression
50
(No Transcript)
51
(No Transcript)
52
- Encounter with antigen can result in the
formation of memory T cells. - Some immunologists have claimed that continuing
re-contact with antigen may be important for the
survival of these memory T cells. - One significant differences between memory T
cells and memory B cells is that the TCR does not
undergo isotype switching or affinity maturation
by somatic mutation, unlike the BCR. - However, it is clear that there are long-lived
CD4 and CD8 cells that are rapidly activated on
contact with antigen.
53
- Memory T cells can be defined by a change in the
expression of certain surface molecules