Borderline Personality Disorder - PowerPoint PPT Presentation
1 / 22
Title:
Borderline Personality Disorder
Description:
Lithium and CBZ for mood stabliisation. transient psychotic symptoms - neuroleptics ... Labile affect. Chronic feelings of emptiness. Uncontrollable anger ... – PowerPoint PPT presentation
Number of Views:170
Avg rating:3.0/5.0
Title: Borderline Personality Disorder
1
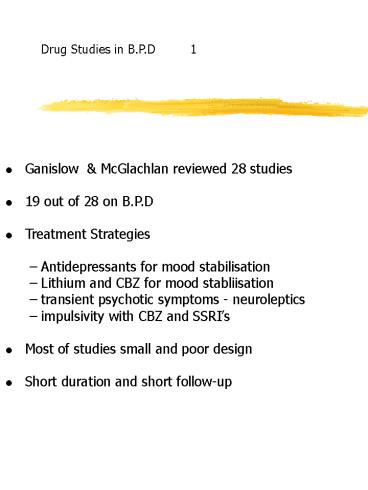
Drug Studies in B.P.D 1
- Ganislow McGlachlan reviewed 28 studies
- 19 out of 28 on B.P.D
- Treatment Strategies
- Antidepressants for mood stabilisation
- Lithium and CBZ for mood stabliisation
- transient psychotic symptoms - neuroleptics
- impulsivity with CBZ and SSRIs
- Most of studies small and poor design
- Short duration and short follow-up
2
Guidelines for Management
- Think of BD not BPD
- Regard the emotional dysregulation and
dyscontrol - behaviours as both biological and learned
- components
- Stick with it but dont overdo it
- Look for change at about ten years
- Treat mood disturbance as actively as you can
- Use brief hospital admissions dont strive not
to admit - Watch out for increasing social isolation as
borderline - symptoms subside
- Have all acute ward staff learn some basic
- DBT techniques
3
Borderline Personality Disorder ?
The concept / diagnostic boundaries The natural
history Drug treatment Other treatment
studies Guidelines for Management
4
Stability of diagnosis / natural history
- Early studies show poor prognosis / outcome
- Borderline syndrome and organisation
- Follow up for 5 years or less
- Pre DSM III
- Prevailing psychoanalytic zeitgeist
- Often defined by treatment failure
- Perjorative Labelling borderline
5
Werble B. Archives Gen. Psych. 1970
- Grinker RR, Werble B and Dryce 1968
- The Borderline Syndrome Basic Books
- N 51
- Follow up 3 - 5 years
- Prospective, inpatient
- No improvement, low functioning, 1/3
re-admitted
6
Paris J Brown, R Nowlis 1987
- Comprehensive Psychiatry 1987 Vol 28
-
1988 Vol 29 - All D.I.B Borderline Personality Disorder
- N 322
- 15 year follow up
- Less impulsivity with time
- 23 re-admitted mainly due to unstable
- social functioning
- Limited pleasurable activities
7
Drug Studies in B.P.D 2
- Soloff - low dose haloperidol
- Gaolberg - low dose thiothixine
- Cowdry - alprazalem
- - carbamazepine
- - trifluperazine
- - tranylcypromine
- Frankenburg - clozapine
- Salzman - fluoxetine
8
Stability of diagnosis / natural history
- 2nd generation studies
- Used Gundersons D.I.B. / DSM III
- Tighter less subjective research designs
- Longer follow up 15 years
9
McGlachlan T.H. Bardenstein KK Archives 1986
- Chestnut lodge study N 89
- Long term outcome of borderline personality
- Arch. Gen. Psych. 1986
- Mean follow up 15 years
- Good outcome increased with time
- Good work functioning
- Suicide rate 3
- Personal stability by avoiding intimacy
10
Drug Studies
Soloff PH. Et al (1993) Efficacy of
phenelzine and haloperidol in borderline
personality disorder Arch. Gen Psych. 1993 50
377 - 85 Cornelius JR et al (1990) Fluoxetine
trial in borderline personality
disorder Psychopharm. Bull 1990 26 151 -
64 Cowdry RW et al (1988) Pharmacotherapy
of borderline personality disorder Arch. Gen
Psych. 45 111 - 9
11
Stone et al The PI 500
- New York State Psychiatric Institute Studies
- N 550 personality dis. 205 Borderline PD
- Follow up 10 - 23 years
- Improvement in functioning after 5 - 10 years
- not before
- Journal of Personality Disorders 1987
12
Drug Studies BPD 3
- Low dose neuroleptics benefit those who have
- ideas of reference, paranoid ideation or
- dissociative reactions to stress
- Alprazolam increases behavioural dyscontrol
- Equivocal or negative results from
- amitriptyline on mood symptoms / increased
dyscontrol - Better results from MAOIs but high
- non - tolerance rate
- Carbamazepine
- decreased behavioural dyscontrol
- improved mood
- better able to tolerate negative
- affect without acting out
- Equivocal results from Fluoxetine
13
Delivery of Acute Care
- Tyrer et al 1994 Psychol. Medicine
- Compared Early Intervention Service (EIS)
- with standard hospital treatment
- EIS Group did better
- 1.2 days inpatient treatment EIS
- 9.3 days standard hospital treatment
- 50 patients had personality disorder
- Personality Disorder patients did better with
- standard hospital care
- - greater improvement in depressive symptoms
- - greater improvement in social functioning
- Linehans studies fit in here
14
Outpatient Treatment
- Perry et al metanalysis of psychotherapy
studies - for personality disorder
- Effect size 1.04 self report
- Effect size 1.13 observer rating
- Require longer courses of psychotherapy
- improvement occurs around 50 sessions
- Patients with least disturbance do best
- particularly with traditional forms of
psychotherapy -
(Paris 1996) - Suicidal behaviour increases in 1st year
- of psychotherapy
(Waldinger 1987) - decreases in years 2 - 5
15
Day patient treatment
- Piper et al 1993 hospital and community
psychiatry - Time limited dynamic group orientated
- 42 drop out rate
- only 14 had Borderline Personality Disorder
- Bateman (In press)
16
Assertive Community Treatment ACT
- In vivo assistance and training of patients
- ACT workers provide care not just broker it
- Staff teamwork emphasis
- High staff patient ratio (caseload N 10)
- ACT lowers treatment costs for non
- schizophrenic psychosis
- Cost for Schizophrenia same
- Costs for Personality Disorders doubled
- - no clear benefit
- Stein Test (Archives 1980)
17
Borderline Personality Disorder
Borderline Personality Disorder 1994 The
Psychiatric Clinics of North America Share I.A.
Ed W B Saunders, Philadelphia Kernbeg O.F.
(1994) Chapter I in above. Aggression, Trauma
and Hatred in the treatment of Borderline
patients pp 701 - 7014 Van der Kolk et al (1994)
Chapter 2 in above. Trauma and the development
of Borderline Personality Disorder pp 715 - 730
18
Borderline Disorder not B.D.P.
- Symptoms and behaviours define it
- No different to severe OCD, Anorexia Nervosa
- Is this the same disorder as complex PTSD
- or Disorder of Extreme Stress ? (DES)
- Not trait based changes with time
19
Borderline Personality Disorder
75 female 2 general population 10 psychi
atric outpatients 30 - 60 psychiatric
inpatients with personality disorder
20
Borderline Personality Disorder DSM IV
- A pattern of instability in personal
relationships, - self image and affects, and marked impulsivity
which - begins by early adulthood
- Fear of abandonment
- Unstable interpersonal relationships
- Disturbance of self identity
- Impulsivity
- Recurrent self harm
- Labile affect
- Chronic feelings of emptiness
- Uncontrollable anger
21
Emotionally unstable personality disorder I.C.D.
10
Impulsive type 3 of 5 criteria borderline
type 3 of impulsive criteria and 2 from
borderline
22
Borderline Personality Disorder Diagnosis
- Validity and reliability of most DSM IV
- Axis II diagnoses close to zero
- Gunderson BPD has higher validity and
- reliability if structured interview used
- BPDs meet criteria for between 4 - 6
- Other Axis II labels
- Why is BPD not in Axis I