Clinical Course - PowerPoint PPT Presentation
1 / 44
Title:
Clinical Course
Description:
YF Liaw (Hepatology, 1984) Anti-HBe appeared in days to years after disappearance of HBeAg ... YF Liaw (Hepatology, 1987) 16 non-cirrhotic Anti-HBe( ) with AE ... – PowerPoint PPT presentation
Number of Views:74
Avg rating:3.0/5.0
Title: Clinical Course
1
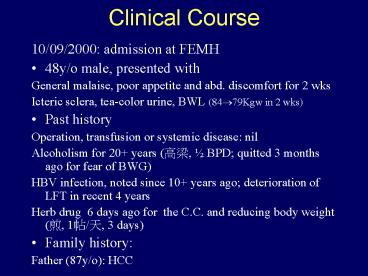
Clinical Course
- 10/09/2000 admission at FEMH
- 48y/o male, presented with
- General malaise, poor appetite and abd.
discomfort for 2 wks - Icteric sclera, tea-color urine, BWL (84?79Kgw in
2 wks) - Past history
- Operation, transfusion or systemic disease nil
- Alcoholism for 20 years (??, ½ BPD quitted 3
months ago for fear of BWG) - HBV infection, noted since 10 years ago
deterioration of LFT in recent 4 years - Herb drug 6 days ago for the C.C. and reducing
body weight (?, 1?/?, 3 days) - Family history
- Father (87y/o) HCC
2
- Lab.
- GOT 1040, GPT 1405, PT 43.7(11.9), Bil. (T/D)
19.3/11.1, ammonia 111 ?M/L, AFP 207 ng/ml - HBsAg(), HBeAg(-), Anti-HBe(), anti-HCV(-)
- Sonography CLPD, no ascites
- Supportive care, including Lamivudine 100mg/day
(starting on 10/11) - Clear consciousness but deteriorated lab.
- For impending hepatic failure, pt was
transferred to NTUH on 10/13/2000
3
- 10/13/2000 admission at NTUH
- Lab.
- HBV DNA 1.47 pg/ml(??PCR, lt0.5 pg/ml),
anti-Delta (-), anti-HAV IgM(-), CMV IgM(-),
EBV-VCA IM(-), HSV (-) - ANA(-), Ceruloplasmin 22.7 mg/dl (-)
- Clinical condition
- Deterioration with ongoing drowsy consciousness,
hyperbilirubinemia, and prolonged PT - Complicated with UGI bleeding
4
- 10/19/2000 transfer to SICU
- Dialysis with Biological DT system for 5 times
- Renal shut down, presented with progressive
decreased urine amount, since 10/21 - B/C grew Candida albican S/C grew MRSA,
Neisseria and Yeast-like organisms then,
strongest antibiotics (Imepinem and Amphotericin
B) were used on 10/25 but sepsis seemed
intractable - Continuous venous-venous hemodialysis was started
on 10/27 for renal failure - Bradycardia and hypotension developed on 11/1 and
then recurred even using high dose of
vasopressors and inotropes - Expire was declared on the same day (11/1)
5
Serial lab. after transfer to SICU
6
48y/o male Alcoholism for 20 years HBV carrier
for 10 years
2wks
General malaise, poor appetite and abd.
discomfort
6 days
Herbs, 3 days use for weight reduction and above
symptoms
Icteric sclera, tea-color urine, BWL (5Kgw in 2
weeks)
At FEMH GOT/GPT, Bil(T), PT, NH3, AFP HBsAg(),
HBeAg(-), Anti-HBe(), Anti-HCV(-) Start
Lamivudine 100mg/day on 10/11 Deterioration of
clinical condition
10/9
10/13
At NTUH, GOT/GPT, Bil(T), PT, AFP HBV DNA 1.47
pg/ml HAV, HDV, CMV, EBV, HSV, ANA,
Wilsons(-) Deterioration with ongoing drowsy
consciousness, ?Bil.,?PT
10/19
At SICU Dialysis with Biological DT system,
5X ARF(CVVH), Sepsis (Fungemia Bacteremia)
Expire
11/1
7
Acute exacerbation
Supportive care Lamivudine
AHF
Herbs
Biological DT system
MOF
ARF Sepsis
Antibiotics CVVH
Death
8
Acute hepatic failureFulminant hepatitis,
fulminant hepatic failure
- Definition by IASL(1996)
- Interval between onset of jaundice and
encephalopathy lt 4 wks - 2 most important complications cerebral edema
and sepsis - Prognostic markers age gt 40 yrs, bilirubin gt 15
mg/dl, PT prolongation gt 25s, cerebral edema (3
or 4 factors, MR gt 90)
9
Liver transplantation
- Urgent LT is now the standard Tx for AHF
- One year survival rate 46-89
- Main problems lack of donor livers and few
qualified centers
10
Alternatives to LT
- Bridge to LT
- Hepatocyte transplantation, liver-directed gene
therapy, xenotransplantation, extracorporeal
liver support, tissue-engineered organs - Using biological DT system, 4/20 survived
(including 2 FHB, 1 flare-up of HBV) - WJ Ko (ISFA, 2001)
11
Acute exacerbation
Supportive care Lamivudine
AHF
Herbs
Biological DT system
MOF
ARF Sepsis
Antibiotics CVVH
Death
12
Alcoholic liver disease
- Fatty liver ? Alcoholic hepatitis ? Cirrhosis ?
Hepatoma - Dose and duration dependent (80g/day for 10 yrs
?) - Risk factors female, viral hepatitis, gene,
nutrition - ??(45) 150 cc/day (YF Liaw TJ Chen, 1992)
(Small 55, 300cc)
13
Alcoholic hepatitis
- GOT/GPT gt 2
- GOT lt 300 IU/dl
- ? Alk-p and ?-GT(15X)
14
ALD and HBV
- Alcohol consumption intensifies the liver disease
caused by HBV - Nomura (AJE, 1988)
- Asymptomatic HBV carriers were at risk of hepatic
abnormalities when drinking more than 80g/day - Villa (Lancet, 1982)
15
More severe Chronic liver injury
Limited illness
Rapid downhill course
Acute Flare-up
HBeAg Clearance
Mutant HBV
Hepatoma
Chronic hepatitis B
Spontaneous reactivation
Hepatitis A
Hepatitis E ?
Drug reaction
Hepatitis C
Corticosteroid Immuosuppressant C/T
Hepatitis D
16
Viral superinfection in chronic HBV carrier
17
Superinfection of hepatitis C
18
Rapid downhill course
Acute Flare-up
HBeAg Clearance
Mutant HBV
Chronic hepatitis B
Drug reaction
19
Natural course of chronic hepatitis B
20
Natural course of chronic hepatitis B
- Indicators of HBV replication
- HBeAg HBV DNA in serum
21
SeroconversionHBeAg(-), Anti-HBe()
- 17 per year male gt female
- Liaw (1983,1984)
- Cessation of HBV replication and clinical
biochemical resolution - Realdi (1980), Hoofnagle(1981), Sanchez(1984)
22
Decompensation in seroconversionIS Sheen
(Gastroenterology, 1985)
- 376 HBeAg(), 7 years
- 165 HBeAg clearance (seroconversion)
- 4 hepatic decompensation (2.42) and one died
23
Window period of seroconversionYF Liaw
(Hepatology, 1984)
- Anti-HBe appeared in days to years after
disappearance of HBeAg - 79 in one year
- 41 in one month
- Shortest is 9 days
- Longest is 3 years
- Shorter in patient with AE
Patient Profile HBeAg(-) Anti-HBe()
24
AFP in hepatitis B with AEYF Liaw (Liver, 1984)
Patient Profile AFP 207
25
Rapid downhill course
Acute Flare-up
HBeAg Clearance
Mutant HBV
Chronic hepatitis B
Drug reaction
26
AE in Anti-HBe() HBV DNA()
- AE in Anti-HBe() vs. HBeAg()
- Incidence/year 10.3 vs. 26.8 (plt0.001)
- Bilirubin and AFP slightly higher in Anti-HBe()
- No significance in S/S, GPT and histology
- 62.5 with HBV DNA () reactivation of HBV
infection - YF Liaw (Hepatology, 1987)
- 16 non-cirrhotic Anti-HBe() with AE
- 88 (14/16) with HBV-DNA() reactivation of HBV
infection - MY Lai (Hepato-gastroenterology, 1988)
27
Detection of HBV DNA
- Real-time Quantitative PCR
- HBV DNA 1.47 pg/ml ( lt 0.5 0.05 pg/ml)
- 30 X of the minimal detectable titer
?????
28
HBV DNA in relation to GPTYF Liaw (Liver, 1988)
29
Role of HBV DNA
- An absence or low levels of circulating HBV DNA
(PCR) in the serum on HBV replication - Hepatocellular injury is a likely sequela of the
host immune response to HBV Ag and is not due to
a direct cytopathic effect of the virus
HBV-DNA pg/ml
0
9
0-250
78
67
251-500
CAHCLH
501-1000
20
8
CM CHU (Hepatology,1985)
gt1000
30
Pre-Core mutants of HBV
- Carman (Lancet, 1989)
- 7 of 8 anti-HBe() HBV DNA() (mostly CAH)
- TGG?TAG (stop codon) (G-to-A substitution at
nucleotide 1896) resulting in failure to produce
HBeAg - Low prevalence in fulminant hepatitis B in France
and North America(lt10) but high in Israel and
Japan (80-100)
31
Pre-Core mutant in TaiwanCM Chu (J Clin
Microbiol, 1996)
Immune tolerance phase Wild type HBV
predominant Immnue clearance phase Precore
mutant emerging Immune integrated phase Precore
mutant prevailing
32
Pre-Core mutants after seroconversionRN Chien
(Spring convention, 2000)
- After spontaneous seroconversion
- 67 remain stable
- 33 have AE
- 70 precore mutant (23 of all)
- 21 re-appearance of HBeAg (5 of all)
33
AFP in hepatitis B with AEYF Liaw (Liver, 1986)
Patient Profile AFP 207
34
Benefit of Lamivudine in AERN Chien (Spring
convention, 2000)
- Hepatitis B with AE (? Bil. PT)
- Lamivudine 150mg/d for 8 weeks
35
Rapid downhill course
Acute Flare-up
HBeAg Clearance
Mutant HBV
Chronic hepatitis B
Drug reaction
36
????????
- ?????
- ??,??,??,??,??,???,???,???,??,??
- ?????
- ??,??,???,??,??,???,??,???,??,??
- ????
- ??,??,??,??,??,??,??
37
?? Scutellariae Radix
- ????
- Liver injuries induced by herbal medicine,
syo-saiko-to (xiao-chai-hu-tang). - Itoh S. (DDS, 1995)
38
??? Moutan Radicis Cortex
- ?????
- Hepatitis induced by traditional Chinese herbs
Possible toxic components. - Kane JA. (Gut, 1995)
39
?? Gentianae Radix
- ?????
- Hepatitis induced by traditional Chinese herbs
Possible toxic components. - Kane JA. (Gut, 1995)
40
Herbal drugs related hepatotoxicity
41
(No Transcript)
42
(No Transcript)
43
Acute exacerbation
Supportive care Lamivudine
AHF
Herbs
Biological DT system
MOF
ARF Sepsis
Antibiotics CVVH
Death
44
(No Transcript)