Hemodynamics in a lobule: a computational model
1 / 1
Title:
Hemodynamics in a lobule: a computational model
Description:
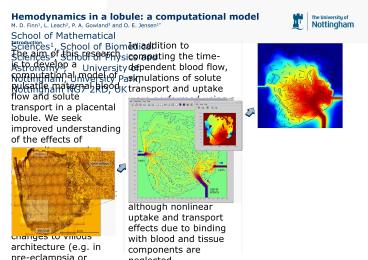
We seek improved understanding of the effects of unsteadiness and villous tree ... The inset shows the instantaneous fluid pressure, with red indicating high ... –
Number of Views:43
Avg rating:3.0/5.0
Title: Hemodynamics in a lobule: a computational model
1
Hemodynamics in a lobule a computational model
M. D. Finn1, L. Leach2, P. A. Gowland3 and O. E.
Jensen1 School of Mathematical Sciences1, School
of Biomedical Sciences2, School of Physics and
Astronomy3, University of Nottingham,
University Park, Nottingham NG7 2RD, UK
Introduction The aim of this research is to
develop a computational model of pulsatile
maternal blood flow and solute transport in a
placental lobule. We seek improved understanding
of the effects of unsteadiness and villous tree
compliance on the flow environment of the villi
and associated nutrient delivery. The model is to
be used to quantify how pathological changes to
villous architecture (e.g. in pre-eclampsia or
diabetes) affect blood flow and solute transfer
efficiency. Existing studies of maternal blood
flow in a lobule have been restricted to
porous-medium models with artificial treatment of
arterial blood jet inertia 1 or to simple
spatially averaged models of blood-villi
interaction 2. Our computational model
presently captures the effects of spatially
resolved time-dependent flow and can be extended
to include a compliant villous structure, solute
transport, and, ultimately, remodeling and growth
of the villous tree. Methods Geometrical data for
our computational work was obtained from
microscope images of villous tree structure. A
slice showing villi between the chorionic plate
and the decidua-basalis from an uncomplicated
pregnancy is shown in Figure 1. The
lattice-Boltzmann computational method 3 was
used to simulate pulsatile blood flow in an
idealized two-dimensional placental lobule based
on our microscope images, as shown in Figure 2.
Large villi are included directly in our
simulations, whilst smaller terminal villi are
represented as a series of line segments (across
which there is no flow) with a density intended
to reflect the actual villi density. An arterial
inlet velocity is prescribed giving a
physiological peak jet Reynolds number of 30 1.
Equal pressure is specified at the two veins.
Artery and vein locations are chosen to provide a
source and sinks for the flow. The positioning is
somewhat arbitrary since the computation is made
in a two-dimensional slice, which in general is
unlikely to intersect actual arteries and
veins. Figure 1 Cross-section
through a lobule between the chorion and
decidua-basalis. A lobule taken from a delivered
placenta was frozen in liquid nitrogen, sliced on
a cryostat, and stained with toluidine-blue to
show the villous tree tissue.
Figure 3 Colour plot
illustrating drop in solute concentration as
solute is uptaken by the villous tree. Red
indicates the high arterial inlet concentration
blue indicates low concentration. Flow in a
two-dimensional slice through each lobule was
visualized using the intravoxel incoherent motion
measurement technique 4 on a low-resolution 3
Tesla system. The ex-vivo perfusion system
produced similar results to existing in vivo
measurements 4. The next stage of the work will
be to use a new 7 Tesla system to obtain
high-resolution images of blood flow that can be
compared directly to the computational
results. Conclusions We have developed a powerful
tool with which to understand important
mechanisms of transport within a placental
lobule. Our approach allows the specification of
the tree geometry and the spatial resolution of
the blood flow field and associated solute
uptake. Preliminary ex-vivo magnetic resonance
imaging of flow in a perfused lobule has been
successful further experiments on a more
powerful scanner should allow us to produce
quantitative flow measurements with which to test
computational predictions. References 1. F. F.
Erian, S. Corrsin and S. H. Davis, J. Biomech.,
10807-814 (1977) 2. H. M. Byrne, P. Gowland, O.
Jensen, T. Mayhew, M. McGuinness, C. Please and
S. Wilson, Proc. 2nd Mathematics-in-Medicine
Study Group, Univ. Nottingham, pp 11-17 (2001) 3.
S. Chen and G. D. Doolen, Annu. Rev. Fluid Mech.,
30329-364 (1998) 4. R. J. Moore, B. Issa, P.
Tokarczuk, K. R. Duncan, P. Boulby, P. N. Baker,
R. W. Bowtell, B. S. Worthington, I. R. Johnson
and P. A. Gowland, Mag. Res. Med., 43295-302
(2000) This work was funded by the UK Medical
Research Council. Corresponding author
oliver.jensen_at_nottingham.ac.uk
In addition to computing the time-dependent blood
flow, simulations of solute transport and uptake
were performed using a finite-difference
technique using a distributed first-order uptake
term. The regime studied is applicable to a range
of solutes (oxygen, carbon-dioxide, glucose,
salts...) although nonlinear uptake and transport
effects due to binding with blood and tissue
components are neglected. Results Figure 2 shows
instantaneous blood flow streamlines at the peak
of an arterial jet. Figure 3 shows an
illustration of how solute dissolved in the blood
is taken up by the villous tree structure as it
is convected through the lobule. Computations
reveal that inertia of the blood jet emerging
from the spiral arteries plays a key role in
delivering solutes deep into the lobule. This is
important because blood solute diffusivities are
relatively small, and therefore villi rely on
convection rather than diffusion for nutrient
delivery. Even with blood inertia, however, it is
found that close to the chorion, where there is a
very slow flow, nutrient delivery is relatively
poor. Figure 2 Screenshot
of lattice-Boltzmann computations, showing the
lobule geometry, instantaneous streamlines of
maternal blood flow at the peak of an arterial
pulse, with the colour indicating flow speed. The
inset shows the instantaneous fluid pressure,
with red indicating high pressure at the artery,
and blue indicating low pressure at the veins.
The predicted pressure drop from artery to vein
is 1 mmHg. The physiological pressure drop would
be greater due to the increased flow resistance
caused by denser packing of terminal
villi. Magnetic resonance imaging To validate the
computational model, magnetic resonance imaging
has been used to image the flow in perfused
delivered placentae. Two peristaltic pumps were
used to perfuse both the maternal and fetal sides
of a lobule using a water based perfusate
containing heparin to prevent clotting.