Non-Invasive Blood Pressure Measurement Techniques - PowerPoint PPT Presentation
1 / 14
Title:
Non-Invasive Blood Pressure Measurement Techniques
Description:
... require annual checks to insure that mechanical wear or shocks haven't ... The VHA's policy is to comply with the EPA's Pollution ... ready? ... – PowerPoint PPT presentation
Number of Views:1076
Avg rating:3.0/5.0
Title: Non-Invasive Blood Pressure Measurement Techniques
1
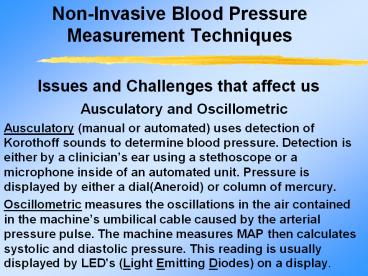
Non-Invasive Blood Pressure Measurement
Techniques
Issues and Challenges that affect us
- Ausculatory and Oscillometric
- Ausculatory (manual or automated) uses detection
of Korothoff sounds to determine blood pressure.
Detection is either by a clinicians ear using a
stethoscope or a microphone inside of an
automated unit. Pressure is displayed by either a
dial(Aneroid) or column of mercury. - Oscillometric measures the oscillations in the
air contained in the machines umbilical cable
caused by the arterial pressure pulse. The
machine measures MAP then calculates systolic and
diastolic pressure. This reading is usually
displayed by LED's (Light Emitting Diodes) on a
display.
2
Which one is better?
Oscillometric Pros and Cons
- Movement,muscle tremors and abnormal heart
rhythms, a very weak pulse or pressure can cause
some automated units to fail to obtain a reading.
- And most devices need a reasonably steady BP
during deflation to accurately detect the
appearance, maximum and disappearance of pressure
oscillations. And the initial price may restrict
its wide spread use. - But they are easily transportable, very easy to
use, can give multi-parameter readings
(temperature, SpO2), can have a built-in paper
recorder, have no observer bias and are
mercury-free. And when used properly give
accurate and repeatable readings.
3
The oscillometric method does not determine the
blood pressure instantaneously but it determines
it from the curves of the changes in the pressure
and its oscillation.This feature has anti-noise
characteristics as it is not affected by external
noise or electric surgical units.
Even when the Korotkoff sounds are hardly
detected due to hypotension, the oscillometric
method is capable of determining BP because the
cuff oscillates as long as the artery pulsation
exists.
4
Which one is better?
Ausculatory Pros and Cons
- Two types of manometers are used in this
facility, Aneroid and Mercury. Aneroids require
annual checks to insure that mechanical wear or
shocks havent affected readings. - Mercury is the Gold Standard of NIBP but needs
accuracy checks as well. - Most of the problems with ausculatory are
operator induced such as digit preference,
observer bias and differences with operators in
auditory acuity. - But now the major problem with mercury manometers
is the mercury used inside the manometers.
5
Whats this I am hearing about getting rid of
mercury?
- The VHAs policy is to comply with the EPAs
Pollution Prevention Act, Resource Conservation
and Recovery Act and all state and local
environmental regulations in controlling and
reducing elemental mercury and mercury containing
compound in the health care waste stream with the
goal of eliminating mercury from the health care
waste stream by 50 by 2005 and eventually
achieving a mercury-free environment. - Locally, we are conducting an inventory to
document the number and types of medical and
non-medical devices containing mercury then where
practical utilize mercury-free products. Also
promoting awareness of the problems associated
with mercury is a large part of the solution.
6
Why do we need to do this?
- Mercury is found in many medical devices and uses
such as thermometers, BP manometers, esophageal
dilators as well as many non-medical products. If
these products are broken, spilled or disposed of
improperly, mercury can be released into the
environment. Incinerators release mercury into
the environment when waste containing mercury is
burned. Hospitals contribute 4-5 of the total
wastewater mercury load. There is up to 50 times
more mercury in medical waste that in general
municipal waste. Mercury from thermometers
contribute about 17 tons of mercury in landfills
annually. - Even if properly recycled its reuse in new
products pose the same eventual risk. Inside the
hospital mercury spills are costly because of the
special training, equipment and disposal
required.
7
Surely Mercury isnt that bad!
Exposure to mercury can occur three ways
inhalation, ingestion and absorption. The most
likely route of inorganic mercury is through
inhalation after a spill.
- Short term exposure to mercury vapor can cause
nausea, shortness of breath, pneumonitis and
bronchitis. Long term exposure can lead to
personality changes, memory loss, stupor and
coma. - The elemental mercury used in thermometers and
manometers is converted by microorganisms in the
environment to methlymercury, the most toxic
form. Exposure to organic mercury is through the
water we drink by contamination of groundwater or
by the food we eat because of contamination of
the environment. - Methlymercury is a neurotoxin and especially
dangerous to fetuses and young children. A 2001
CDC study found that 10 of women have mercury
levels high enough to cause neurological damage
to their children.
8
Wouldnt keeping mercury out of the environment
make these questions easier to answer?
Is this fish mercury-free?
Has mercury contaminated this lake?
9
What do I do if I think my equipment is not
working properly?
- The most common problems affect both ausculatory
and oscillometric types. - First make sure that you dont have an external
air leak either in the cuff or tubing connecting
the cuff to the unit. Aging BP cuffs are the
source of most air leaks replacements are
available from SPD (both single and dual tube
types). - If you suspect a mechanical or electronic problem
then call the work order desk at extension 5018.
The more information (type of unit , problems
experienced) you can provide will speed up any
repairs.
10
What Affects A Reading?
No matter which method you use there are common
issues that affect both methods of measuring
blood pressure. First the equipment
- Is the cuff you are using sized for the patient?
A cuff too large can cause reading to be lower
than actual and a cuff too small can cause
reading to be higher than actual. - Cuff sizes areSmall Adult 17-25cm/Standard Adult
23-33cm/Large Adult 31-40cm/Thigh 38-50cm. - Is the equipment (either sphygmomanometer or
vital signs monitor) working properly? Air leaks
in the cuff, tubing or inside the unit can affect
the deflation rate. - An mercury or aneroid manometer that is
improperly zeroed will affect the entire reading.
11
How does the patients state affect the pressure
reading?
- Is your patient ready?
- If your patient has finished a cigarette or an
alcoholic beverage within the last 15 minutes the
readings will be altered. - If they havent sat quietly for at least 5
minutes or are talking during the procedure, the
readings will be altered. - And if you have placed the cuff over a shirt
sleeve the readings will not be reliable.
12
What can I do to insure an accurate reading?
- Follow the Hypertension guidelines for BP
measurement. - Daily before using any type of manometer verify
that it is in good working order. - And if you feel that the device you are using is
not providing an accurate reading, tag the device
and notify the work order desk at extension 5018.
13
My Critikon wont take a BP reading!!
Is it the cuff OR Is it the Critikon??? Connect
each one of the cuffs to the Critikon, push start
and see what happens!
14
Whats Your Rate? Deflation that is...
Inflate the cuff to 200mm/Hg Tell the timer to
start the clock, then deflate the cuff at the
recommended 2-3 mm/sec rate. After 20 seconds
when the timer says stop, close the valve. We
tell you what your rate is!