Needlestick Safety and Prevention Act - PowerPoint PPT Presentation
Title:
Needlestick Safety and Prevention Act
Description:
(last line of defense) T. R. A. I. N. I. N. G. In order of preference. Types of Safety Features ... consultation if viral resistance suspected. HIV PEP for ... – PowerPoint PPT presentation
Number of Views:1208
Avg rating:3.0/5.0
Title: Needlestick Safety and Prevention Act
1
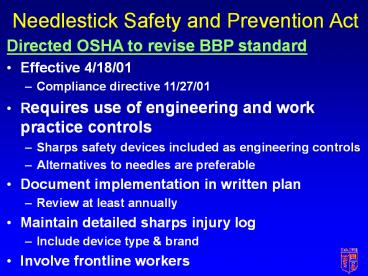
Needlestick Safety and Prevention Act
- Directed OSHA to revise BBP standard
- Effective 4/18/01
- Compliance directive 11/27/01
- Requires use of engineering and work practice
controls - Sharps safety devices included as engineering
controls - Alternatives to needles are preferable
- Document implementation in written plan
- Review at least annually
- Maintain detailed sharps injury log
- Include device type brand
- Involve frontline workers
2
Bloodborne PathogensExposure Control Plan
- Statement of employer policy
- Designation of responsible employees
- Determination of employee exposures
- Implementation
- Standard (universal) precautions
- Engineering controls
- Work practices controls
- Personal protective equipment
- Training
- Hepatitis B immunizations
- Implementation
- HB surveillance (optional)
- Post-exposure evaluation and follow-up
- Housekeeping
- Labeling
- Mandated use of needles and other sharps with
integrated safety features - Safety Device Evaluation Committee
- Documentation of waivers
- Recordkeeping and reporting
3
HBV Preexposure Prophylaxis
- Recombinant DNA vaccine available since 1986
- From yeast cells
- Subunit HBsAg
- 1.0 ml IM given at 0, 1 and 6 months
- Accelerated 0, 1, 2 and 12 months
- For HCWs, document immunity anti-HBS 2-6 months
post-vaccination - 6 doses maximum
- Once immune, no boosters
4
Recordkeeping Rule
- Effective 1/1/02
- New OSHA forms 300 log, 300A summary and 301
incident report - Expanded general recordkeeping requirements
- May use new log for recording contaminated sharps
injuries if - Record all data required, including brand
- Able to segregate sharps info from log for
privacy concerns
5
Joint Commission on Accreditation of Healthcare
Organizations
- Preventing Needlestick and Sharps Injuries -
Sentinel Event Alert, Issue 22, August 2001 - Cites and reviews NIOSH Alert and the Needlestick
Safety and Prevention Act. - In April 2002, JCAHO will begin assessing
organizational compliance with the new provisions
of the Needlestick Safety and Prevention Act.
6
- The prevention of occupational diseases is
primarily the function of the industrial
management, secondarily, the function of the
plant physician. In an ideal industrial
establishment the two work together the
physician is conversant with all the processes of
manufacture and is therefore able to link up the
disturbances of health he observes among the
workers with the processes in which they are
engaged. He cooperates with management in the
effort to introduce safeguards .... He is,
however, in a subordinate position and therefore
the prime responsibility in the prevention of
occupational disease lies with the management,
which has the last word in regard to methods of
work, substances used, and equipment for the
prevention of disease. - Alice Hamilton, MD Harriet L. Hardy, MD
- Industrial Toxicology, 1949
7
Prevention of Work-related BBP Infection
Haddon, 1970
8
Controlling Exposures
In order of preference
T R A I N I N G
- Substitution
- Isolation or enclosure
- Ventilation (general/dilution local exhaust)
- Work and hygiene practices
- Personal protective equipment
- (last line of defense)
9
Types of Safety Features
Chiarello, 1995
10
Design Features of a Safer Needle Device
- Barrier between hands and needle after use
- Allow or require workers hands to remain behind
needle at all times - Integral part of device and not accessory
- Be in effect before disassembly and remain in
effect after disposal - Be simple, self-evident to operate and require
little or no training
FDA, 1992, 1995
11
Click for larger picture
12
MMWR 1/17/97
13
Recommended Personal Protective Equipment
YYes, NNo, M1Yes if splashing likely, M2Yes
if soiling likely, M3At certain times
CDC 1989
14
Management of Occupational Blood Exposures
- Provide immediate care to the exposure site
- Wash wounds and skin with soap and water.
- Flush mucous membranes with water.
- Determine risk associated with exposure by
- Type of fluid (e.g., blood, visibly bloody fluid,
other potentially infectious fluid or tissue, and
concentrated virus) and - Type of exposure (i.e., percutaneous injury,
mucous membrane or nonintact skin exposure, and
bites resulting in blood exposure).
15
Management of Occupational Blood Exposures
- Evaluate exposure source
- Assess risk of infection using available
information. - Test known sources for HBsAg, anti-HCV, and HIV
antibody (consider using rapid testing). - For unknown sources, assess risk of exposure to
HBV, HCV, or HIV infection. - Do not test discarded needles or syringes for
virus contamination.
16
Management of Occupational Blood Exposures
- Evaluate the exposed person
- HBV immune status
- Tetanus prophylaxis
- Baseline lab tests for HCV, HIV, chemistry
profile, complete blood count, urinalysis,
pregancy test PRN - Give PEP for exposures posing risk of infection
transmission
17
HBV Postexposure Prophylaxis
- Always indicated unless
- Documented immune
- Waiver signed
18
Hepatitis B Virus Postexposure Prophylaxis
Click for larger picture
19
HCV Postexposure Prophylaxis
20
HIV Postexposure Prophylaxis
- Depends on
- Type of exposure
- Severity
- Volume
- Source HIV status
- Prophylactic treatment
- May not be warranted
- Basic regimen
- Expanded regimen
21
HIV Infection Status
- HIV-Positive Class 1
- Asymptomatic
- Known low viral titer, lt1500 RNA copies/ml
- HIV-Positive Class 2
- Symptomatic
- AIDS
- Acute seroconversion
- Known high viral load
22
Selected HIV PEP Regimens
- BASIC REGIMEN
- Zidovudine (Retrovir ZDV AZT) Lamivudine
(Epivir 3TC) available as COMBIVIR - ZDV 600 mg per day, in 2 or 3 divided doses
- 3TC 150 mg twice daily
- EXPANDED REGIMENBasic regimen plus
- Indinavir (Crixivan IDV)
- 800 mg every 8 hours, on an empty stomach
23
Recommended HIV Postexposure Prophylaxis for
Percutaneous Injuries
CDC. MMWR 2001.
24
Recommended HIV Postexposure Prophylaxis for
Mucous Membrane and Non-intact Skin Exposures
CDC. MMWR 2001.
25
Reported Failure of Combination Drug PEP to
Prevent HIV Infection in HCWs Exposed to
HIV-Infected Blood
26
Management of Occupational Blood Exposures
- Initiate HIV PEP as soon as possible, preferably
within 2 hours of exposure - Offer pregnancy testing to all women of
childbearing age not known to be pregnant - Seek expert consultation if viral resistance
suspected - HIV PEP for 4 weeks if tolerated
27
Management of Occupational Blood Exposures
- Provide counseling
- Emotional effects
- Risks of transmission
- Medications, including adherence
- Advise exposed persons to seek medical evaluation
for any acute illness occurring during follow-up - Perform follow-up testing
- Monitor for adverse effects
- Seroconversion
28
Sample Protocol for Follow-up if on HIV PEP
Medications
29
Primary Side Effects of Antiretroviral Agents
30
Compliance with HIV PEP
N449 subjects with follow-up at 4-6 weeks
HIV PEP Registry, 3/31/99
31
Reasons HIV PEP Discontinued
N197
HIV PEP Registry, 3/31/99
32
Management of Occupational Blood Body Fluids
Exposures
- Summary
- Provide immediate care to the exposure site.
- Determine risk associated with exposure.
- Evaluate the exposed person.
- Give PEP for exposures posing risk of infection
transmission. - Provide counseling.
- Perform follow-up testing.
33
Resources