Infections of Bone and Joint - PowerPoint PPT Presentation
1 / 46
Title:
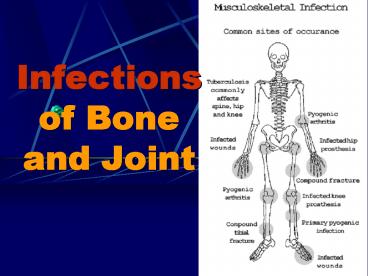
Infections of Bone and Joint
Description:
By this time, sinus or sequestrum formed, the disease has reached the chronic stage. ... The sinus closed and the infection subsided. X-ray findings ... – PowerPoint PPT presentation
Number of Views:3424
Avg rating:3.0/5.0
Title: Infections of Bone and Joint
1
Infections of Bone and Joint
2
Osteomyelitis
3
Introduction
- Osteomyelitis is an inflammation of bone caused
by an infecting organism. - It may remain localized, or it may spread through
the bone to involve the marrow, cortex,
periosteum, and soft tissue surrounding the bone. - The term is only applied to the infection caused
by pyogenic bacteria not including inflammation
of TB.
4
Classification
- Attempts to classify osteomyelitis have been
based on - (1) the duration and type of symptoms
- (2) the mechanism of infection
- (3) the type of host response to the infection.
- Based on the duration and type of symptoms,
osteomyelitis may be acute, subacute, or chronic
5
Classified according to mechanism
- Osteomyelitis may be
- exogenous
- hematogenous.
- The exogenous form is an infection caused by
trauma, surgery (iatrogenic), or a contiguous
infection. - The hematogenous form may result from known or
unknown bacteremia.
6
Periosteal medullits???
- The infection may involve the marrow spaces,
Haversian canals and subperiosteal space. When
all the bony components are involved, it means. - Staphylococcus Aureus is the most common
etiologic agent, causative bacteria or causal
organisms. - Today we also pay attention to the infection of
Staphylococcus Epidermidis, the gram-negative
anaerobic bacilli.
7
Organisms may reach the bone by one of following
3 paths
- 1)directly through a skin wound which
communicated with the bone, usually as a
complication of the open fracture, and it is not
often present as acute process.
8
Organisms may reach the bone by one of following
3 paths
- 2)directly spread from a neighboring soft tissue
infection or adjacent infective focus - 3)indirectly via the blood stream, - Hematogenous
spread. - The blood stream is invaded from a minor
abrasion or boil (furuncle), sore throat,
gingivitis. It intends to be more acute.
Hematogenous spread is the most common route of
infection by far.
9
Acute hematogenous osteomyelitis
- From any focus of infection, organisms often
enter the blood stream to form the temporary
bacteremia, but they can not survive in the major
of cases. - If they reach an area that the vitality of the
tissue is lower than normal, they may multiply
and reproduce.
10
Acute hematogenous osteomyelitis
- Although the normal bone has an excellent blood
supply, there is slowing of the circulation in
the metaphyseal region. - Acute hematogenous osteomyelitis occurs most
frequently in meduallary cavity of long bones and
in children usually begin in the metaphysic.
11
The pathogenic organisms easily settle in the
metaphysis at the growing end of long bone
possibly because
- 1.knee is liable to be injuried, traumatic
hematomas is a suitable medium for bacteria
growth. - 2.the more rapidly the bone grows, the more blood
supply is. In long bone, the growing end has more
blood flow, the hairpin arrangement of
capillaries has slowed down the rate of blood
flow. - 3.the rapid growing cells are susceptible
affected by traumatic infection. Metaphysis is
the relative lack of phagocytes, so the upper end
of the tibia and the lower end of the femora are
the most commonly infected part.
12
Pathological change
- organisms enters , blocks, settles, multiply
- Hyperemia (congestion) tension builds up
- Exudates, a suboeriosteal abscess.
- it spreads, re-enter the bone, deprived of its
blood supply. - forced down the medullary canals, destroying the
marrow blood supply
13
(No Transcript)
14
Pathological change
- The cortex may be surrounded externally and
internally by pus and deprival of its blood
supply. - As a result, unless the early evacuation of the
pus, a segment of bone dies and eventually
separates to form a sequestrum. - The bone dies when its blood supply is cut off by
infective thrombosis. The nutrient artery to
endanger large area of the diaphysis, - liable to
pathological fracture.
15
Pathological change
- The importance of early decompression.
- Eventually the abscess bursts through the
periosteum into the soft tissue. - Perforation, and along fascial planes.
- Finally, it may through the skin to the surface
and form a chronic sinus becoming a persistent
sinus tract or cloaca. - By this time, sinus or sequestrum formed, the
disease has reached the chronic stage.
16
(No Transcript)
17
Clinical features history
- The onset is rapid and attacks in short time.
- The patient, usually a child or adolescent,
- complains a severe pain in a limb, and the pain
is not relieved by rest. - A complete history and physical examination are
required to search for possible primary foci of
infection. There may be some minor injury or
insignificant infective lesion such as boil sore
throat a few days earlier.
18
The general symptoms of toxemia
- ?severe acute illness appear
- ?irritable and restless
- ?high fever, chill
- ?rapid pulse, nausea, vomiting etc
19
local signs
- caloric, rubor, dolor, tumor
- Heat, red, pain or tenderness, swelling
- Initially, the lesion is within the medually
cavity, there is no swelling, soft tissue is also
normal. - The merely sign is deep tenderness.
- Localized finger-tip tenderness is felt over or
around the metaphysic. - it is necessary to palpate carefully all
metaphysic areas to determine local tenderness,
pseudoparalysis
20
Subperiosteal abscess formation
- Edematous, red and fluctuation
- indicating subperiosteal abscess formation.
- As the subperiosteal abscess formed, signs of
inflammation followed rapidly. - The extremity is held in semiflexion,
- surrounding muscles are in spasm
- passive movement is resisted
21
Clinic pictures
- An increase effusion in the adjacent joint proves
in most cases to be a sympathetic synovitis with
sterile clear fluid. Hydroarthrosis should not be
confused with septic arthritis. - It is important to remember that the metaphysis
lie within the joint capsule of the hip,
shoulder, ankle. Therefore these joints can
develop septic arthritis by extension of
osteomyelitis. - If the infection and septicemia proceeded
unabated, the patient may have toxic shock
syndrome.
22
Laboratory findings
- The white blood cell count will show a marked
leulocytosis as high as 20,000 or more - The blood culture demonstrates the presence of
bacteremia, the blood must be taken when the
patient has a chill, especially when there is a
spiking temperature. - Aspiration. The point of maximal tenderness
should be aspirated with a large-bore needle. - The thick pus may not pass through the needle.
- Any material aspirated should be gram stained and
cultured to determine the sensitivity to
antibiltics.
23
X-ray findings
- x-ray films are negative within 1-2 weeks,
- Although carefully comparison with the opposite
side may show abnormal soft tissue shadows. - It must be stressed that x-ray appearances are
normal in the acute phase. There are little value
in making the early diagnosis. - by the time there is x-ray evidence of bone
destruction, the patient has entered the chronic
phase of the disease.
24
Bone scans
- Radioisotopic bone scaning was valuable in early
localization(within 48 h) of bone infection.
- The specificity of radioactive isotopic imaging
techniques have improved in the evaluation of
musculoskeletal infection. - Tc99m imaging is very sensitive , it is the
choice for acute hematogenous osteomyelitis, the
overall accuracy was 92.
25
Prompt diagnosis
- The acute infection of bones can be cured by
prompt appropriate antibiotic therapy. - Bone and joint show special problems for the host
defense mechanism because of its rigid structure.
- Once pus forms under pressure, the vascular
supply is lost, resulting in areas of infected ,
devitalized bone. - Septic emboli in bone or vascular thrombosis can
cause additional devascularization. - Antibiotics can inhibit or cure an infection only
when they can reach the infecting organisms. - Infections producing pressure in a bone as well
as relatively avascular tissues can impede or
prevent antibiotics from reaching the primary
site of infection.
26
Prompt diagnosis
- Unfortunately the time between initial infection
and circulatory embarrassment is often rather
short (perhaps as early as 72 hours after the
beginning of infection). - Even under the best of circumstances, if
treatment is undertook lately the end result
might be the loss or abnormal function. - The early diagnosis and rapid initial treatment
is extremely important.
27
Early diagnosis depends on fllowings
- 1. severe acute illness, rapid onset and toxemia
- 2. local severe pain and unwillingness to move
limbs - 3.deep tenderness
- 4.WBC count is as high as 20,000 or more
- 5.every effort must be made to obtain a bacterial
culture and determinate the sensitivity to
antibiotics - Tc99m scaning
- CT or MRI
28
Differential diagnosis
- 1. soft tissue infection such as cellulitis, deep
abscess - 2.acute suppurative/septic arthritis
- 3.Rheumatic fever less acute, polyarticular
involvement, increased ASO - Ewings sarcoma x-ray shows onion-peel bone
deposition
29
Treatment
- ! 1.general treatment nutritional therapy or
general supportive treatment by intaking enough
caloric, protein, vitamin etc. - 2. antibiotics therapy
- 3.surgical treatment
- 4.immobilization
30
antibiotics therapy
- early, large dosage, sensitive and continued
- The prompt administration of antibiotics is so
vital that the result need not be waited, usually
using wide-spectrum antibiotics, even by
intravenous administration during the first 1-3
days. - The choice of antibiotics may subsequently be
modified according to culture, sensitivity
results, and clinical response. - The treatment should be continued for at least 2
weeks after the body temperature is down to the
normal in order to minimize the possibly of
reoccurrence.
31
surgical treatment
- Pressure exerted by pus enclosed within a rigid
compartment is tremendous. - Circulation of the bone is destroied, antibiotics
can not reach the organism and there will has
extensive necrosis of bone, - As any infection in a closed space, immediate
provision of drainage is of paramount importance.
- This must be done at earliest possible
opportunity even before signs of subperiosteal
abscess is evident. - To wait is to invite disaster.
32
surgical treatment
- Surgery is indicated if an abscess is present
regardless of the clinical course. It is
indicated when there has been no response to
vigorous antibiotics treatment after 48-72 hours.
- Surgery is achieved by making a skin incision
over the most tenderness site, dividing the
peristeum and opening the medullary cavity using
either a series of drill holes or gauging out a
window in the bone cortex to decompress rather
than debridement.
33
immobilization
- when the infected area is immobilized,
- the patient is more comfortable
- relieving pain
- to treat the infection by resting the limbs and
ensue the healing process. - If the damage to the bone is significant, cast
immobilization may be important to prevent a
pathologic fracture, remains for many weeks. - If the damage to articular cartilage is
suspected, traction might prevent further
destruction but still allow joint mobility. In
acute osteomyelitis of the upper femur, traction
is needed to prevent hip dislocation.
34
Treatment
- It is very difficult to provide a permanent cure
for chronic osteomyelitis, most antibiotics fail
to penetrate the barrier of fibrous tissue plus
bone sclerosis. - Chronic osteomyelitis presents quite different
problem from the acute form. Its primary problem
is surgical removal of all dead and poor
vascularized tissues. - If this is properly done under appropriate
antibiotic therapy, the operation must be
carefully planed as it often means significant
removal of bone and surrounding tissues. - Since the introduction of local muscle flap
procedures, the success rate is 93 with local or
vascularized flap, debridement and antibiotics.
35
Chronic osteomyelitis
- If any of sequestrum, abscess cavity, sinus tract
or cloaca is present. - Hematogenous infection with an organism of low
virulence may be present by chronic onset. - Infection introduced through an external wound
usually causing a chronic osteomyelitis. - It is due to the fact that the causative organism
can lie dormant in avascular necrotic areas
occasionally becoming reactive from a flare up.
36
Clinical features
- During the period of inactivity, no symptoms are
present. - Only Skin-thin, dark, scarred, poor nourished,
past sinus, an ulceration that is not easily to
heal - Muscles-wasting contracture, atrophy
- Joint-stiffness
- Bone-thick, sclerotic,
- often contain abscess cavity
37
Clinical features
- At intervals, a flare-up occurs,
- The relapse is often the result of poor body
condition and lower resistance. - A lighting up of infection is manifested by
aching pain that is worse at night. - Locally there will be some heat, swelling,
redness,tenderness, edema, because pus may build
up in cavity,then a sinus may open and start to
exudates purulent materials and small sequestra. - The sinus closed and the infection subsided.
38
X-ray findings
- In the early stage, the bone appears at
moth-eaten change and osteoporosis, then
sclerosis develops. - The periosteum is elevated by subperiosteal
lamination of new bone which becomes thick and
dense progressively.
39
Treatment
- It is very difficult to provide a permanent cure
for chronic osteomyelitis, most antibiotics fail
to penetrate the barrier of fibrous tissue plus
bone sclerosis. - Chronic osteomyelitis presents quite different
problem from the acute form. Its primary problem
is surgical removal of all dead and poor
vascularized tissues. - If this is properly done under appropriate
antibiotic therapy, the operation must be
carefully planed as it often means significant
removal of bone and surrounding tissues. - Since the introduction of local muscle flap
procedures, the success rate is 93 with local or
vascularized flap, debridement and antibiotics.
40
Septic arthritis
- The most common - Staphylococcus aureus.
- The hips and knees are the most frequently
affected sites. - Route of infection
- Hematogenous spread from an infective focus
- Spread from an adjacent focus
- Direct introduction by the wound
41
Pathology
- 1. serous arthritis
- Synovium is congested, edematous and
infiltrated with WBC. Synovial fluid increased in
the amount with clear or slight opaque appearance
and slight amount WBC - 2. serofibrinous
- arthritis-fibrin is
excessive - 3. purulent arthritis synovium-inflammation
is more intense, areas of vascular thrombosis and
local necrosis occurjoint fluid-WBC 2-5105/mm3,
opaque, thick gray or yellowish in colourthe
prolytic enzymes dissolve the articular
cartilage, even erode the bone---fibrous
ankylosis
42
Diagnosis
- If a joint is suspected of being infected,
aspiration with a large-bore needle should be
performed promptly and before antibiotic therapy
is begun. - Careful skin preparation before aspiration is
mandatory, and the fluid obtained should be sent
for immediate Gram staining, culture, cell
counts, and crystal analysis.
43
3 essential principles in the management
- (1) the joint must be adequately drained,
- (2) antibiotics must be given to diminish the
systemic effects of sepsis - (3) the joint must be rested in a stable
position. - Prompt, adequate evaluation of purulent joint
fluid appears to be crucial both for preservation
of articular cartilage and for resolution of the
infection.
44
Treament
- If the diagnosis is made early and the involved
joint is superficial, such as the elbow or ankle,
aspiration should be performed and repeated if
necessary, appropriate antibiotics should be
administered, the joint should be splinted in a
position of function, and the patient should be
observed for a decrease in pain, swelling, and
temperature and for improved joint mobility.
45
Treament
- Initial antibiotic treatment is empirically based
on the patients age and the risk factors. - Empirical antibiotic therapy should be used until
culture and sensitivity results are available. - Although some infections clear up within 7 days,
antibiotic regimens often should be continued for
4 to 6 weeks, depending on the clinical course.
46
Treament
- As the infection resolves, therapy to restore
normal joint function is begun, including
functional splinting initially to prevent
deformity, isometric muscle strengthening, and
active range-of-motion exercises. - Patients being treated for infectious arthritis
often have varying degrees of deformity, and
treatment with traction, dynamic splints, serial
casting, and passive exercises may be useful.