Role of surgery - PowerPoint PPT Presentation
1 / 54
Title:
Role of surgery
Description:
Alternatively, gastrojejunostomy with truncal vagotomy is also an option. Postoperative Complications for Peptic Ulcer surgery Early complication : ... – PowerPoint PPT presentation
Number of Views:145
Avg rating:3.0/5.0
Title: Role of surgery
1
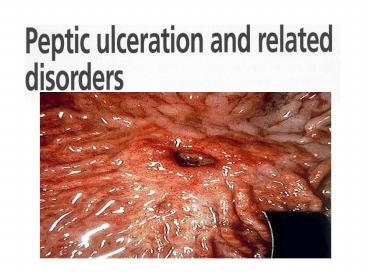
(No Transcript)
2
Introduction
3
Role of surgery
- Despite advances in medical therapy to inhibit
acid secretion and to eradicate H. pylori,
surgery remains important in managing these
patients. Over the last 2 decades, there has been
an increase in emergency operations performed for
complications of peptic ulcers while the number
of operations for elective indications has
decreased markedly. - An ulcer by definition extends through the
muscularis mucosa in contrast to an erosion,
which is superficial to the muscularis mucosa.
4
Etiologies of Duodenal ulcer
- Duodenal ulcer disease is a disease of multiple
etiologies. The only absolute requirements are
secretion of acid and pepsin in conjunction with
either H. pylori infection or ingestion of
NSAIDs.
5
Etiologies of gastric ulcers
- Most of gastric ulcers appear to behave more like
duodenal ulcers and are associated with excess
acid. - Types I and IV gastric ulcers are defects in
mucosal protection - types II and III are associated with acid
hypersecretion and behave like duodenal ulcers - Gastric cancers ( suspicious ) may ulcerate and
resemble gastric ulcers. - Furthermore, ulcers may be caused by nonacid or
other peptic disorders such as Crohns disease,
syphilis, Candida infection, or malignant
diseases such as Kaposis sarcoma, lymphoma,
carcinoma, or pancreatic carcinoma.
6
Clinical Manifestations
- Young and middle-aged patients
- Pain or one of complication ( perforation ,
bleeding , obstruction pyloric obstruction ,
hour glass stomach , penetration , malignant
transformation in gastric ulcer )
7
ABDOMINAL PAIN
- The most common symptom is mid-epigastric
abdominal pain that is usually well localized.
The pain is usually tolerable and frequently
relieved by food. Moreover, the pain may be
episodic, may be seasonal in the spring and fall,
or may relapse during periods of emotional
stress. For these reasons and because it is
relieved, many patients do not seek medical
attention until they have had the disease for
many years. - When the pain becomes constant, deeper
penetration of the ulcer, and referral of pain to
the back is usually a sign of penetration into
the pancreas. - Diffuse peritoneal irritation is usually a sign
of perforation.
8
PERFORATION
- Acute Vs subacute
- Pathology 3 Stages
- Sudden sever abdominal pain ,assosiated with
neusia and vomiting , and variable degree of
shock - Peritonitis , frequently accompanied by fever,
tachycardia, dehydration, and ileus . - Abdominal examination reveals tenderness,
rigidity, and rebound. - A hallmark of perforation is the demonstration
of free air underneath the diaphragm on an
upright chest radiograph. This complication of
duodenal ulcer disease represents a surgical
emergency. Once the diagnosis is made, operation
should be performed in an expeditious fashion
following appropriate fluid resuscitation.
9
BLEEDING
- The most common cause of death in patients with
peptic ulcer disease is bleeding in patients who
have major medical problems or are older than 65
years of age. - Because the duodenum has an abundant blood supply
and the gastroduodenal artery lies directly
posterior to the duodenum bulb. - Most duodenal ulcers present with only minor
bleeding episodes that are detected by the
presence of Melina
10
OBSTRUCTION
- Gastric outlet obstruction manifested by delayed
gastric emptying, anorexia, or nausea accompanied
by vomiting. - In cases of prolonged vomiting, patients may
become dehydrated and develop a hypochloremic,
hypokalemic metabolic alkalosis. Fluid
resuscitation requires replacement of the
chloride and potassium deficiencies in addition
to nasogastric suction for relief of the
obstructed stomach. - In addition to acute inflammation leading to
functional gastric outlet obstruction , chronic
inflammation of the duodenum may lead to
recurrent episodes of healing followed by repair
and scarring with ultimately fibrosis and
stenosis of the duodenal lumen. In this
situation, the obstruction is accompanied by
painless vomiting of large volumes of gastric
contents with similar metabolic abnormalities as
seen in the acute situation. The stomach can
become massively dilated in this setting, and it
rapidly loses its muscular tone. Marked weight
loss and malnutrition are also common in this
situation.
11
Gastric Ulcer
- Like duodenal ulcers, gastric ulcers are also
characterized by recurrent episodes of quiescence
and relapse. They also cause pain, bleeding, and
obstruction and can perforate. Hemorrhage occurs
but the most frequent complication is
perforation. Most perforations occur along the
anterior aspect of the lesser curvature. Similar
to duodenal ulcer, gastric outlet obstruction can
also occur.
12
Zollinger-Ellison syndrome
- Zollinger-Ellison syndrome is a clinical triad
consisting of gastric acid hypersecretion, severe
peptic ulcer disease, and non-beta islet cell
tumor of the pancreas. The tumors are known to
produce gastrin and are referred to as
gastrinomas.
13
(No Transcript)
14
Diagnosis
- History and physical examination
- Upper GIT endoscopy
- A serum gastrin level should also be obtained in
patients with - ulcers that are refractory to medical therapy or
require surgery. - An upright chest radiograph is usually performed
when ruling out perforation. - H. pylori testing should also be done in all
patients with suspected peptic ulcer disease.
15
HELICOBACTER PYLORI TESTING
- Serology is the test of choice for initial
diagnosis when endoscopy is not required. - If, however, endoscopy is to be performed, the
rapid urease assay or histology are both
excellent options. - After treatment (only if necessary) the urea
breath test is the method of choice
16
Treatment
- Medical Management with exceptions
17
Surgical Procedures for Peptic Ulcer Disease
- VAGOTOMY
- TRUNCAL and drainage procedures
- SELECTIVE VAGOTOMY
- HIGHLY SELECTIVE VAGOTOMY
- Gastrectomy
18
Types of VAGOTOMY
19
Heineke-Mikulicz pyloroplasty Vs
gastro-jejunostomy should be associated with
truncal vagotomy or selective vagotomy but not
highly selective vagotomy
20
Hemigastrectomy with Billroth 1 (gastroduodenal)
anastomosis
21
Hemigastrectomy with Billroth II
GASTROJUJINOSTOMY
22
LAPAROSCOPIC PROCEDURES
- Both parietal cell vagotomy and posterior truncal
vagotomy with anterior seromyotomy (Taylor
procedure) can be accomplished laparoscopically
and represent effective antiulcer operations.
23
Surgical Indications
- It salvages patients from life-threatening
complications associated with perforation,
hemorrhage, and gastric outlet obstruction.
24
Approach to the Patient Bleeding from Peptic
Ulcer Disease
- Approximately 80 of upper gastrointestinal
bleeds are self-limited. - The initial step in management is adequate
initial and on going resuscitation. - Following resuscitation, endoscopy is performed
to assess the cause and severity of the bleed. - Mortality increases with age ,the severity of the
initial bleed is also an adverse prognostic
factor, and this might include the presence of
shock, a high transfusion requirement, or bright
red blood in the nasogastric tube or in the
stool. Recurrent bleeding, concomitant disease
increased the mortality rate. Also Visible
vessel was seen during endoscopy
25
- Endoscopy remains the investigation of choice for
patients with upper gastrointestinal bleeding
from peptic ulcer disease. - Not only for diagnosis but also therapy.
- When the bleeding is controlled, long-term
medical therapy includes antisecretory agents
usually in the form of a proton-pump inhibitor
plus testing for H. pylori, with treatment if
positive. - If H. pylori is present, documentation of
eradication should be performed following
therapy. If the bleeding continues or recurs,
surgery may be indicated.
26
Treatment of Bleeding Duodenal Ulcers
- For those patients who continue to bleed or who
are referred by the endoscopist , the duodenal
bleeding is usually controlled by opening the
duodenum and oversewing the ulcer with a U stitch
from the vessel, which is usually the
pancreaticoduodenal artery or gastroduodenal
artery. - As most of these patients are elderly, have bled
a significant amount, and have some degree of
hypotension, the more time-consuming parietal
cell vagotomy is usually not performed. Instead,
a truncal vagotomy with pyloroplasty is performed.
27
(No Transcript)
28
Bleeding Gastric Ulcers
- For bleeding gastric ulcers, a distal gastrectomy
with Billroth I anastomosis is usually performed.
29
Perforated Duodenal Ulcers
- Simple patching of a perforated duodenal ulcer
followed by medical treatment is all that is
necessary for patients who present with a
perforated duodenum secondary to peptic ulcer
disease. Patch closure of the duodenum can be
performed by either a laparoscopic or open
procedure.
30
(No Transcript)
31
Perforated Gastric Ulcer
- For perforated gastric ulcers that occur in
hemodynamically stable patients, distal
gastrectomy with Billroth I reanastomosis is
usually performed. - However, simple patching of the gastric ulcer,
testing for H. pylori, and treatment if positive
can also be considered. However, the risk of
malignancy needs to be ruled out therefore,
biopsy of the ulcer bed also needs to be
performed.
32
Gastric Outlet Obstruction
- The first principle is to categorize the patient
as either acutely or chronically obstructed. - If the patient is acutely obstructed, the
patient should be treated nonoperatively with
nasogastric decompression, intravenous fluid,
nutritional support as needed, and acid
suppressive therapy. H. pylori should be tested
for and treated. - if the patient has chronic gastric outlet
obstruction operative therapy is usually
indicated to open up the gastric outlet. In
addition, an acid-reducing procedure is
necessary.
33
Preoperative
- Nasogastric decompression for several days.
- Correction of fluid and electrolyte imbalances.
- Antisecretory therapy.
- Endoscopy with biopsies.
34
Operative
- Gastrectomy can be done if technically feasible.
- Alternatively, gastrojejunostomy with truncal
vagotomy is also an option.
35
Postoperative Complications for Peptic Ulcer
surgery
- Early complication bleeding , stomal
obstruction , duodenal blow-out - Postgastrectomy Syndromes Secondary to Gastric
Resection( Dumping SYNDROME, METABOLIC
DISTURBANCES,AFFERENT LOOP - and EFFERENT LOOP SYNDROME)
- Postvagotomy Syndromes
36
Postgastrectomy Syndromes
- DUMPING SYNDROME
- Dumping syndrome refers to a symptom complex that
occurs following ingestion of a meal when a
portion of the stomach has been removed or the - normal pyloric sphincter mechanism has become
disrupted. - Dumping syndrome exists in either a late or an
early form, with the early form occurring more
frequently.
37
EARLY DUMPING
- The early form of dumping syndrome usually occurs
within 20 to 30 minutes following ingestion of a
meal . - The gastrointestinal symptoms include nausea and
vomiting, a sense of epigastric fullness,
eructations, cramping abdominal pain, and often
explosive diarrhea. - The cardiovascular symptoms include
palpitations, tachycardia, diaphoresis, fainting,
dizziness, flushing, and occasionally blurred
vision. - This occurs because gastrectomy or interruption
of the pyloric sphincteric - mechanism prevents the stomach from
preparing its contents and delivering them to the
proximal bowel in the form of small particles in
isotonic solution. The resultant hypertonic food
bolus passes into the small intestine, which
induces a rapid shift of extracellular fluid into
the intestinal lumen to achieve isotonicity. - Following this shift of extracellular fluid,
luminal distention occurs and induces the
autonomic responses listed earlier. - Dietary measures are usually sufficient to manage
these patients.
38
LATE DUMPING
- Appears 2 to 3 hours after a meal.
- The basic defect in this disorder is also rapid
gastric emptying. When carbohydrates are
delivered to the small intestine, they are
quickly absorbed, resulting in hyperglycemia that
triggers the release of large amounts of insulin
to control the rising blood sugar. This results
in an actual overshooting such that a profound
hypoglycemia occurs in response to the insulin.
This activates the - adrenal gland to release catecholamines,
which results in diaphoresis, tremulousness,
lightheadedness, tachycardia, and confusion. - The symptom complex is indistinguishable from
insulin or hypoglycemic symptom . - These patients should be advised to ingest
frequent small meals and to reduce their
carbohydrate intake.
39
METABOLIC DISTURBANCES
- Anemia
- Iron deficiency anemia a combination of decreased
iron intake, impaired iron absorption, and
chronic subclinical blood loss secondary to the
hyperemic, friable gastric mucosa primarily
involving the margins of the stoma where the
stomach connects to the small intestine. In
general, the addition of iron supplements to the
patients diet corrects this metabolic problem.
- Megaloblastic anemiaVitamin B12 deficiency
occurs secondary to poor absorption ,due to lack
of intrinsic factor secretion . The patient
should be treated with intramuscular injections
of cyanocobalamin every 3 to 4 months
indefinitely.
40
METABOLIC DISTURBANCES
- Impaired absorption of fat. On occasion,
steatorrhea may be seen after gastrectomy and
Billroth II reconstruction as a result of
inadequate mixing of bile salts and pancreatic
lipase with ingested fat because of the duodenal
bypass. - Deficiency in fat-soluble vitamins may also
occur. - In the setting of steatorrhea, pancreatic
replacement enzymes are often effective in
decreasing fat loss.
41
METABOLIC DISTURBANCES
- Both osteoporosis and osteomalacia have also been
observed following gastric resection and appear
to be caused by deficiencies in calcium.
42
AFFERENT LOOP SYNDROME
- Usually occurs when the afferent limb is longer
than 30 to 40 cm and has been anastomosed to the
gastric remnant in an antecolic fashion. - Following obstruction of the afferent limb, there
is an accumulation of pancreatic and
hepatobiliary secretion within the limb,
resulting in its distention. - Pancreatic and hepatobiliary secretion occur in
response to ingestion of food, accumulation of
these secretions results in distention, which
causes epigastric discomfort and cramping. In the
setting of partial obstruction, the intraluminal
pressure increases to forcefully empty its
contents into the stomach, resulting in bilious
vomiting that is often projectile but offers
immediate relief of symptoms. There is no food
contained within the vomitus. - If the obstruction has been present for a long
period, it can also be aggravated by the
development of the blind loop syndrome. - For both forms of afferent loop syndrome, acute
and chronic, operation is indicated because it is
a mechanical problem, not a functional problem.
43
EFFERENT LOOP OBSTRUCTION
- The most common cause of efferent loop
obstruction is herniation of the limb behind the
anastomosis in a right-to-left fashion. - Operative intervention is almost always necessary
and consists of reducing the retroanastomotic
hernia and closing the retroanastomotic space to
prevent recurrence of this condition.
44
POSTVAGOTOMY DIARRHEA
- Approximately 30 or more of patients suffer from
diarrhea after gastric surgery. For most
patients, it is not severe and usually disappears
within the first 3 to 4 months. For some
patients, the diarrhea is part of the dumping
syndrome. However, vagotomy is also associated
with alterations in stool frequency - Most patients with postvagotomy diarrhea have
their symptoms resolve over time. In those
patients who fail to resolve their symptoms,
cholestyramine, an anionic exchange resin that
absorbs bile salts and renders them unabsorbable
and inactive, can significantly diminish the
severity of diarrhea.
45
STRESS GASTRITIS
- Stress gastritis has been referred to as stress
ulcerations, stress erosive gastritis, and
hemorrhagic gastritis. - These lesions may lead to life-threatening
gastric bleeding and by definition occur after
physical trauma, shock, sepsis, hemorrhage,
respiratory failure, or severe burns. - They are characterized by multiple, superficial
(non ulcerating) erosions that begin in the
proximal or acid-secreting portion of the stomach
and progress distally. - They may also occur in the setting of central
nervous system disease such as that seen with a
Cushing ulcer or as a result of thermal burn
injury involving more than 30 of the body
surface area (Curling ulcer).
46
Gastric Adenocarcinoma
- H pylori infection increases the risk of gastric
cancer - Morphologic types ulcerating (15), polypoid
(25), superficial spreading (15), linitis
plastica (10), advanced (35) - Symptoms and signs include postprandial
abdominal heaviness early anorexia, with weight
loss vomiting, often with blood, if pyloric
obstruction occurs epigastric mass in 25
hepatomegaly in 10 stool positive for occult
blood in 50 but melena in a few cases - Signs of distant spread metastases to the neck
(Virchow node) or umbilicus (Sister Mary Joseph
node), metastases anterior to rectum detectable
on rectal examination (Blumer shelf), metastases
to ovaries (Krukenberg tumors) - Laboratory findings carcinoembryonic antigen
is elevated in 65 - higher levels indicate extensive spread of tumor
- Endoscopy usually identifies gastric carcinomas
.
47
Treatment
48
Haematemesis
- GI bleeding is any blood loss from the GI tract
(from the mouth to the anus), which may present
with haematemesis, melaena, rectal bleeding or
anaemia. - Haematemesis is defined as vomiting blood and is
usually caused by upper GI disease. - Melaena is the passage PR of a black
treacle-like stool that contains altered blood,
usually as a result of proximal bowel bleeding.
49
Haematemesis
- Haematemesis is usually caused by lesions
proximal to the duodenojejunal junction. - upper GI lesions can cause frank PR bleeding if
sever - Most tumours more commonly cause anaemia than
frank haematemesis. - In young adults, peptic ulcer disease (PUD)and
varices are the common causes. - In the elderly, tumours, PUD and angiodysplasia
are the common causes.
50
Gastric causes
- Erosive gastritis may follow alcohol or NSAID
intake/stress, history of dyspeptic symptoms. - Gastric ulcer possible herald smaller bleeds,
accompanied by altered blood (coffee grounds),
history of PUD. - Gastric cancer anaemia commoner, associated
weight loss, anorexia, dyspeptic symptoms. - Gastric leiomyoma (rare)
- Dieulafoys disease (rare) younger patients,
large bleed.
51
Duodenal causes
- Duodenal ulcer past history of duodenal ulcer,
symptoms of back pain, hunger pains, NSAID use. - Aortoduodenal fistula (rare) usually infected
graft post AAA repair, massive haematemesis and
PR bleed, usually fatal. - Cancer ampula of Vater
52
Esophageal causes
- Bleeding varices sudden onset, painless, large
volumes, dark red blood, history of (alcoholic)
liver disease, physical findings of portal
hypertension. - Reflux oesophagitis associated with
regurgitation. - Oesophageal carcinoma (rare) scanty,
blood-stained debris, rarely significant volume,
associated with weight loss, anergia,dysphagia. - Trauma during vomiting (MalloryWeiss
syndrome) bright red bloody vomit usually
preceded by several normal but forceful vomiting
episodes.
53
General (systemic causes)
54
MANAGEMENT
- Resuscitation
- Minor bleed observation, scheduled OGD ,monitor
haemoglobin . - Major bleed Continued resuscitation, urgent OGD
- VaricesEndoscopic therapy, Sengstaken
tube.,Surgery - Peptic ulcer Endoscopic therapy or surgery
- I.V. PPI treatment, correction of coagulation
profile , protect aganest hepatic coma if LCF is
present - Early feeding