Respiratory tract anatomy - PowerPoint PPT Presentation
1 / 44
Title:
Respiratory tract anatomy
Description:
Respiratory tract anatomy fig 13-1 Conducting zone vs. respiratory zone Conducting zone functions Alveolar structure 1 Alveolar structure 2 Alveolar structure 3 ... – PowerPoint PPT presentation
Number of Views:137
Avg rating:3.0/5.0
Title: Respiratory tract anatomy
1
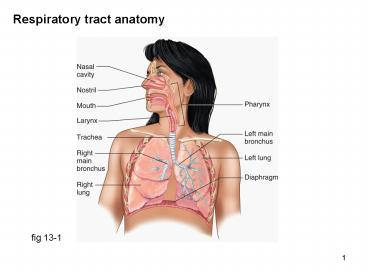
Respiratory tract anatomy
fig 13-1
2
Conducting zone vs. respiratory zone
fig 13-2
3
Conducting zone functions
Regulation of air flow trachea bronchi held
open by cartilaginous rings smooth muscle in
walls of bronchioles alveolar
ducts sympathetic NS epinephrine ? relaxation
(? receptors) ?? air flow leukotrienes
(inflammation allergens ?? leukotrienes ??
mucus constriction) Protection mucus escalator
(goblet cells in bronchioles ciliated
epithelium) inhibited by cigarette smoke Warming
humidifying inspired air expired air is 37?
100 humidity (loss of 400 ml pure
water/day) Phonation larynx vocal cords
4
Alveolar structure 1
fig 13-3b
5
Alveolar structure 2
fig 13-4a
6
Alveolar structure 3
fig 13-4b
7
Alveolar structure (notes)
Type I epithelial cells thin, flat gas
exchange Type II epithelial cells secrete
pulmonary surfactant ?? pulmonary compliance
(later) Pulmonary capillaries completely
surround each alveolus sheet of
blood Interstitial space diffusion distance for
O2 CO2 is less than diameter of red blood
cell Elastic fibers secreted by fibroblasts into
pulmonary interstitial space tend to collapse
lung
8
Lung pressures
Lungs are inflated by being pulled
open Transmural/transpulmonary pressure
Palveolar Ppleural 0 (-5) 5 mm Hg
9
Lung pressures during quiet ventilation
10
Lung pressures during ventilation
Purple line alveolar pressure (Palv) -1 mm Hg
during inspiration 1 mm Hg during
expiration Green line pleural pressure
(Pip) -4 mm Hg at functional residual
capacity -7 mm Hg after inspiration Ptp is
transpulmonary (transmural) pressure i.e. Palv
Pip (e.g. at 2, -1 (-5) 4 mm Hg Lower curve
(black) labeling accidentally omitted x axis
should read 4 sec i.e. time y axis is tidal
volume 500 ml
11
Pleural pressure during ventilation
Quiet ventilation pleural pressure (Pip) always
negative as lung expands, Pip becomes more
negative because recoil (collapsing) force
increases as lung stretches Forced
ventilation Pip negative during inspiration
more negative as lung expands Pip can be
positive during forced expiration (e.g. FEV1
measurement)
12
Airway resistance
Transpulmonary pressure as lungs expand, pleural
pressure becomes more negative transpulmonary
pressure (alveolar pressure pleural pressure)
increases alveoli expand, bronchioles expand ??
airway resistance result inhalation lowers
resistance, exhalation increases
resistance Lateral traction alveoli
bronchioles all interconnected expansion of
lungs stretches alveoli bronchioles ??
resistance net stocking metaphor
13
Lung compliance
Definition ease of expansion e.g. balloon is
compliant, auto tire is less compliant i.e. tire
requires much greater pressure increase to
expand compliance ? volume / ?
pressure Factors that decrease compliance surface
tension of fluid lining alveolar
surface elastic tissue in alveolar
walls expansion of lungs (stretched lungs are
less compliant) Factors that increase
compliance pulmonary surfactant secreted by type
II alveolar cells reduces surface tension of
alveolar fluid mixture of phospholipid and
protein low levels in premature infants
(respiratory distress syndrome)
14
Airway resistance
Epinephrine relaxes bronchiolar smooth muscle
(?2 receptors) Leukotrienes released during the
inflammatory response contract bronchiolar
smooth muscle important in asthma bronchitis
15
Lung volumes
Learn in laboratory tidal volume, inspiratory
reserve volume, expiratory reserve volume,
residual volume, functional residual capacity,
vital capacity, total lung capacity can be
measured with a spirometer FEV1 forced vital
capacity in 1 second (80) Functional residual
capacity lung volume when all muscles are
relaxed (or subject is dead) lung volume at the
end of quiet expiration tendency of lungs to
collapse tendency of thoracic cavity to
expand pleural pressure is negative ( -4 mm Hg)
16
Alveolar ventilation
Minute ventilation tidal volume (ml/breath) x
respiratory rate (breaths/min) Anatomic dead
space space in respiratory tract where no gas
exchange occurs
fig 13-20
17
Alveolar ventilation
fresh air entering lung with each breath tidal
volume dead space Alveolar ventilation
rate (tidal volume dead space) x respiratory
rate Example calculations
respiratory rate tidal volume dead space alveolar ventilation rate
14 /min 500 ml 150 ml 4.9 L/min
24 /min 300 ml 150 ml 3.6 L/min
see also table 13-5
18
Partial pressures
Daltons law In a mixture of gases, each gas
behaves independently and exerts a pressure
proportional to its concentration in the gas
mixture For example Air is 79 N2, 21 O2, 0.4
CO2 Air pressure 760 mm Hg (dry air at sea
level) P.N2 600 mm Hg, P.O2 160 mm Hg,
P.CO2 0.3 mm Hg Partial pressure in solution
partial pressure in gas mixture after
equilibration with solution Why use partial
pressures? because gases diffuse down their
partial pressure gradients (in gas or in
solution)
19
Partial pressures at various sites
fig 13-22
20
Partial pressure solubility
because P.O2 plasma P.O2 blood, putting them in
contact, separated by O2 permeable membrane ? no
net diffusion
21
Alveolar gas composition as AVR varies
Hypoventilation ? alveolar ventilation
rate Hyperventilation ? alveolar ventilation rate
22
Ventilation (air flow) perfusion (blood flow)
matching
If air flow to an alveolus is blocked alveolar
gas venous blood (P.O2 40 mm Hg, P.CO2 45 mm
Hg) The ? P.O2 signals constriction of blood
vessels (hypoxic vasoconstriction) i.e. dont
send blood to an alveolus with no air flow If
blood flow to an alveolus is blocked alveolar
gas atmospheric air (P.O2 160 mm Hg, P.CO2 0
mm Hg) The ? P.CO2 signals constriction of
bronchioles i.e. dont send air to an alveolus
with no blood flow
23
Ventilation (air flow) perfusion (blood flow)
matching
24
Alveolar O2 ? pulmonary capillary blood
fig 13-24
Diseased lung pulmonary edema, interstitial
fibrosis
25
Hemoglobin structure
4 subunits (left) form 1 hemoglobin Iron is
ferrous form (Fe) Hb 4 O2 ? Hb(O2)4
(saturated) deoxyHb oxyHb
fig 13-26
26
Oxygen-hemoglobin dissociation curve
fig 13-27
27
Oxygen-hemoglobin dissociation curve (notes)
100 saturation is when every Hb has 4 O2s
bound Sigmoid (S-shaped) curve indicates that
binding of the 1st O2 increases the affinity of
the other Hb binding sites for O2 (an allosteric
effect technically known as positive
cooperativity) Sigmoid curve means that the
curve is steepest in the region of unloading O2
i.e. in the tissues where P.O2 is lt 40 mm Hg A
steep curve means that a small reduction in P.O2
?? O2 unloaded Curve is flattest in the lung
where P.O2 is 100 mm Hg A flat curve means that
a large reduction in P.O2 ?? reduction in O2
saturation of Hb (e.g. at high altitude or in
diseased lung) Also, flat curve means breathing
100 O2 adds little O2 to the blood
28
O2-Hb curve effect of pH, CO2, DPG, temperature
In working tissue, ? pH, ? P.CO2, ? temperature,
? DPG DPG is diphosphoglycerate (now known as
bisphosphoglycerate) DPG is ? in hypoxic tissue
(and in stored blood in blood banks)
29
O2 from alveolus ? red blood cell in the lung
all O2 movement is by simple diffusion down its
partial pressure gradient
fig 13-29
30
O2 from rbc Hb ? cells
all O2 movement is by simple diffusion down its
partial pressure gradient highest P.O2 in
alveolus lowest P.O2 in mitochondria
fig 13-29
31
CO2 from tissues ? blood
CO2 transport 60 plasma HCO3- 30 carbamino
hemoglobin 10 dissolved CO2 CA carbonic
anhydrase H2O CO2 ? H2CO3
fig 13-31a
32
CO2 from pulmonary blood ? alveolus
CO2 transport 60 plasma HCO3- 30 carbamino
hemoglobin 10 dissolved CO2 CA carbonic
anhydrase H2O CO2 ? H2CO3
fig 13-31b
33
Hemoglobin as a buffer
Notes on next slide
fig 13-32
34
Hemoglobin as a buffer (notes)
In tissues CO2 (produced by metabolism) H2O ?
H2CO3 ? H HCO3- Hemoglobin becomes more basic
when it is deoxygenated, i.e. it binds H more
tightly In the lung Hemoglobin is oxygenated,
becomes more acidic, (i.e. it is a more powerful
H donor), and releases its H H HCO3- ? H2CO3
? H2O CO2 (released into alveolus)
35
Rhythmical nature of breathing
Respiratory rhythm generator located in medulla
oblongata of brainstem During quiet
breathing Inspiration action potentials burst
to diaphragm inspiratory intercostals Expiratio
n no action potentials elastic recoil of lungs
(passive process) During forced breathing (e.g.
exercise, blowing up a balloon) Active
inspiration expiration Expiration with
expiratory intercostals abdominal
muscles Breathing is also modulated by centers in
pons of brainstem lungs
36
Control of ventilation (chemoreceptors)
peripheral chemoreceptors in carotid aortic
bodies
Central chemoreceptors in medulla (brain
interstitial fluid) Stimulated by 1. ? P.CO2
(via ? pH most important) Peripheral
chemoreceptors see left (arterial
blood) Stimulated by 1. ? P.CO2 (via ? pH) 2. ?
P.O2 3. ? pH
fig 13-33
37
Control of ventilation (? arterial P.O2)
fig 13-34
Acts on peripheral chemoreceptors (? P.O2
depresses central chemoreceptors) relatively
insensitive (potentiated by ? P.CO2) responds to
P.O2, not O2 content (i.e. not to anemia or CO
poisoning)
38
Control of ventilation (? arterial P.O2)
fig 13-35
39
Control of ventilation (? P.CO2)
Acts on central peripheral chemoreceptors centr
al chemoreceptors are the most important
regulators of ventilation acts via ? H
(?pH) note sensitivity
fig 13-36
40
Control of ventilation (? P.CO2)
fig 13-37
41
Control of ventilation (? pH)
fig 13-38
? P.CO2 acts via ? pH, but this is ? pH from
other sources (e.g. lactic acid)
42
Control of ventilation (? pH)
fig 13-39
43
Increased ventilation exercise
You would think that exercise ?? AVR by ? CO2, ?
O2, or ? pH However
fig 13-41
44
Increased ventilation exercise possible
mechanisms
fig 13-43
Also axon collaterals from descending tracts to
respiratory centers feedback from joints
muscles