CML CML vs Leukemoid Reaction Chronic Lymphocytic - PowerPoint PPT Presentation
1 / 33
Title:
CML CML vs Leukemoid Reaction Chronic Lymphocytic
Description:
... CML CML vs Leukemoid Reaction Chronic Lymphocytic Leukemia Elderly age Anemia, fever & bleeding slow over years. Lymphocytosis & Lymphadenopathy Spleen, ... – PowerPoint PPT presentation
Number of Views:3148
Avg rating:3.0/5.0
Title: CML CML vs Leukemoid Reaction Chronic Lymphocytic
1
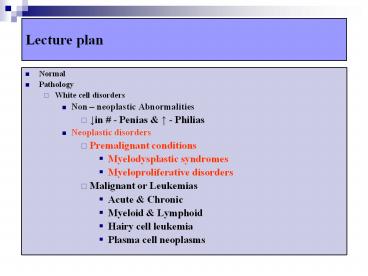
Lecture plan
- Normal
- Pathology
- White cell disorders
- Non neoplastic Abnormalities
- ?in - Penias ? - Philias
- Neoplastic disorders
- Premalignant conditions
- Myelodysplastic syndromes
- Myeloproliferative disorders
- Malignant or Leukemias
- Acute Chronic
- Myeloid Lymphoid
- Hairy cell leukemia
- Plasma cell neoplasms
2
Myelodysplastic Syndromes
- Group of Clonal stem cell disorders
- Characterized by
- Maturation defect ? Ineffective Hematopoiesis
- ?risk of Acute Myeloid Leukemias (AML)
- Types
- Primary or Idiopathic gt 50yrs, Gradual in
onset, - risk of AML ?
- Rx ( RT or Drugs) related (t MDS) after 2 -8 of
RX, complication of Rx, Higher risk of AML (? ?
?) - Pathogenesis
- Unknown
3
Myelodysplastic Syndromes
- Cytogenetic abnormalities
- Deletions (5q,7q,20q), Monosomy (5 7), Trisomy
(8) - Morphology
- Marrow usually Hypercellular,
- Erythroid precursors - ring Sideroblasts, budding
nucleated cells, - Granulocytic Megaloblastoid, Pseudo Pelger
Huet neutrophils( two nuclear segments), - Megakaryocytes- Pawn ball type( multinucleate)
- Peripheral Blood Cytopenias ( Pancytopenia)
- Patients present with Refractory Anemias (not
responding to hematenics even after 6 months of
Rx )
4
Myelodysplastic Syndromes
- FAB classification
- RA Refractory Anemia (Blasts lt1)
- RARS RA with Ring Sideroblasts (lt1)
- RAEB RA with excess blasts (lt5)
- RAEB in T RAEB in transformation (gt5)
- Clinically
- Anemia- weakness
- Leukopenia- Infection ( sore throat)
- Thrombocytopenia- Hemorrhages (patechae, Purpura)
5
MDS - Dysplastic Erythroblasts
6
MDS - Ring Sideroblast
7
Myeloproliferative Disorders
- Disorders of multipotent progenitor cells (
myeloid Lymphoid precursor) - Increased, Functionally abnormal cells.
- Extramedullary hemopoiesis - Organomegaly
- End stage
- Progress to Leukemia
- Myelofibrosis
- Classification
- Polycythemia rubra vera (PV)
- Essential Thrombocythemia (ET)
- Myelofibrosis (MF)
- Chronic Myeloid Leukemia (CML)
8
MDS MPD
- MDS
- Myeloid cells
- Marrow Hypercellular ( can be normal or hypo
also) - Peripheral Cytopenias
- Risk of Acute Leukemia
- Organomegaly may not
- No Spent phase
- MPD
- Mostly Myeloid also Lymphoid cells
- Marrow Hypercellular
- Peripheral Philias or cytosis
- Risk of Acute Leukemia
- Organomegaly (splenomegaly)
- Spent phase (Fibrosis)
9
PV - Natural History
- Indolent
- ?Hgb, Hct ? ?blood viscosity ?Thrombosis (DVT)
- lt 25 progress to ?
- Marked BM fibrosis (spent phase)
- Acute leukemia (2-15)
- Rx of symptoms (i.e. phlebotomy)
10
Essential Thrombocythemia
- ? platelets - episodic symptoms
- Bleeding /
- thrombosis
- infections
- Acute leukemia
- (lt 1)
11
Myelofibrosis
12
Myelofibrosis - Natural History
- Initial cellular phase
- Progressive BM fibrosis / failure
- Infection
- Hemorrhage
- Acute leukemia
- (lt 10)
13
Lecture plan
- Normal
- Pathology
- White cell disorders
- Non neoplastic Abnormalities
- ?in - Penias ? - Philias
- Neoplastic disorders
- Premalignant conditions
- Myelodysplastic syndromes
- Myeloproliferative disorders
- Malignant or Leukemias
- Acute Chronic
- Myeloid Lymphoid
- Hairy cell leukemia
- Plasma cell neoplasms
14
(No Transcript)
15
Leukemia Classification
- Acute Leukemias
- Acute Myeloid Leukemia - AML
- AML M0, M1, M2, M3, M4, M5, M6 M7
- Acute Lymphoid Leukemia - ALL
- ALL - L1, L2 L3 - maturity
- Chronic Leukemias
- Chronic Myeloid Leukemia- CML
- Chronic Lymphoid Leukemia - CLL
16
Leukemias
17
Blasts
18
Acute Leukemia
- Untreated - patients survive lt6 months
- Age predominance
- ALL - children (peak- 4 yrs)
- AML - adults (median age 50 yrs)
19
ALLCervical Lymphadenopathy
20
Organomegaly
21
ALL-Acute Lymphocytic Leuk.
- Common in Children.
- FAB classification L1, L2 L3(PAS- )
- Pre B cell type common.
- Growth failure, Fever, Anemia Lymphadenopathy,
bleeding. - Moderate Hepatosplenomegaly
- tdt CALLA (CD 10) Positive
- Reservoir- Brian Testes
22
AML-Acute Myeloid Leukemia
- Adults common ( 15 39 yrs age)
- FAB classification - M0 to M7.
- Anemia, Fever, Bleeding
- Hepatosplenomegaly moderate
- No significant lymphadenopathy
23
Myeloblasts Myeloperoxidase (MPS) positive
24
AML3- Acute Promyelocytic Leukemia
- Hypergranular promyelocytes
- Increased Auer rods
- DIC from tissue thromboplastin
- 1517 chromosomal translocation
- (retinoic acid receptor gene)
25
AMLM3 - Auer Rods
26
AML-M5 - Gum Hypertrophy
27
AML 5 Non-specific Esterase
AML 5
Control
28
AML - summary
- Mo- undifferentiated, Ultra structurally
Myeloblasts - M1- No maturation, /gt3Blasts MPO ve
- M2- MC(30-40), Auer rods, t(821)
- M3- APML, many Auer rods/cell, Younger age ( 35
yrs), DIC, t(1517) - M4- Myelomonocytic, NSE ve, inv(16)
- M5- Monocytic (MPO-Neg, NSE-Pos), older pts,
Organomegaly, Lymphadenopathy, Tissue
infiltration ( skin- Chloromas), - M6- Erythro, older age, 20 of Rx related AMLs
- M7- Megakaryocytic- Myelofibrosis
29
Chronic Myeloid Leukemia
- Middle age 40-60y
- Philadelphia chromosome, t(922)
- c-abl (Abelson) chromosome 9 bcr (break point
cluster region) chromosome 22 ?Protein with
tyrosine kinase activity - plays - Anemia, Fever Bleeding
- Marked Leukocytosis gt50,000 (abnormal)
- Marked splenomegaly, Hepatomegaly
- Clinical course
- progressive ? accelerated phase ? 80 blast
phase (AML or ALL)
30
CML
31
(No Transcript)
32
CML vs Leukemoid Reaction
33
Chronic Lymphocytic Leukemia
- Elderly age
- Anemia, fever bleeding slow over years.
- Lymphocytosis Lymphadenopathy
- Spleen, liver enlargement
- Common B cell
- Spectrum of disease
- CLL-Blood
- SLL ( Small cell lymphocytic lymphoma)- Lymph node