Enzyme Inhibition Mathews et al. pages 383388 - PowerPoint PPT Presentation
1 / 40
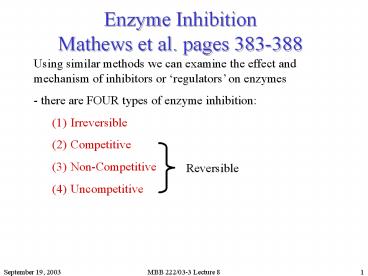
Title: Enzyme Inhibition Mathews et al. pages 383388
1
Enzyme InhibitionMathews et al. pages 383-388
Using similar methods we can examine the effect
and mechanism of inhibitors or regulators on
enzymes - there are FOUR types of enzyme
inhibition (1) Irreversible (2) Competitive (3) N
on-Competitive (4) Uncompetitive
2
Irreversible inhibition
- a compound interferes with the active site so
as to disable it - commonly it is done by the
inhibitors forming a stable covalent adduct with
the enzyme -e.g. renders Ser ineffective -may
also block substrate access to site - many bind
well because they resemble transition states
(TSAs) (eg Sarin) -almost all are toxic substances
Diisopropyl Fluorophosphate (DIFP)
Example of DIFP inactivating chymotrypsin
3
Reversible inhibitionEffect of inhibitors on
the reaction scheme
k1
E S ES E P
kcat
k-1
I
ki
k-i
Ki is the inhibition constant
EI
Ki E I
EI
In some cases, the inhibitor lookslike the
substrate and binds to active site, but it cannot
react like substrate.
4
Competitive inhibition
When an unreactive molecule can bind reversibly
to an enzymes active site and compete with the
substrate to bind enzyme
This form of inhibition causes the Vmax to
remain unchanged the Km to increase measured Km ?
Kmapp Increased substrate can overcome a
competitive inhibitor
5
Figure 11.19 Competitive inhibition
6
Figure 11.21
Inhibitors - a molecule can just resemble the
substrate with a modification where a critical
atom is replaced to prevent the reaction to
occur The example shown here has a -O- replaced
with a -CH2- moiety . The rest of the molecule
is intact so it can make the same interactions
with the enzyme as does the substrate
7
So what does this have do to about observations
of how the enzyme behaves in solution?
-with a fixed I - with a competitive inhibitor
in the reaction we observe an increase in KM
which we call Kmapp. - no effect is seen on Vmax
- on a Lineweaver-Burke Plot, lines intercept on
the Y axis _at_ 1/Vmax
Figure 11.20
8
Non-Competitive Inhibition
Consider an inhibitor that binds to the enzyme,
but not at the active site. In this case the
inhibitor is not competing for the active site -
this binding distorts the enzyme and reduces its
activity this is a case of allosteric
regulation of the enzyme This form of inhibition
causes Vmax to drop Km remains unchanged
increased substrate cannot overcome a
non-competitive inhibitor
9
Figure 11.22 Non-Competitive Inhibition
10
- with a non-competitive inhibitor in the
reaction we observe an drop in Vmax which we call
Vmaxapp. -no effect is seen on Km.
On a Lineweaver-Burke Plot, lines intercept on
the X axis _at_ -1/KM
Figure 11.23
11
Uncompetitive inhibition
- substrate binding to enzyme is not inhibited
- binding of inhibitor to ES complex occurs
(i.e., after S is bound)
- ESI complex is stabilized relative to ES
complex so Km is decreased
- ESI complex is non-productive so Vmax is
decreased and this is not reversed by addition of
more substrate
12
Cooperative substrate binding by allosteric
enzymes
Fig. 11.32
- this can occur in enzymes with more than one
subunit and more than one active site.
- low affinity for substrate
TENSE state
T State
- high affinity for substrate
- occupation at one site influences change in all
sites
R State
RELAXED state
13
Protein Function 2
- Storage and transport molecules
14
Role of Globins in Oxygen Transport Storage
Myoglobin Hemoglobin
15
Myoglobin (Mb) Hemoglobin (Hb)
Proteins involved in STORAGE and TRANSPORT of
oxygen (O2) - how to get O2 from lungs to
cells? PO2 partial pressure of O2
-need to pick up O2 in the lungs (high PO2) -
release in capillaries (moderate to low PO2) -
store until required
PO2
P50 the PO2 where 50 of the heme sites are
filled (have bound O2)
16
Affinities for oxygen
Hemoglobin Moderate affinity Myoglobin High
affinity
During Pregnancy The FETUS must get O2 from the
mothers blood- stream. Here, a special (fetal)
hemoglobin binds O2 with a higher affinity than
adult hemoglobin
17
Hemoglobin - tetramer 2 alpha, 2 beta subunits -
moderate affinity for O2 - sensitive to pH,
CO2 and BPG - binds 4 O2
Myoglobin - monomer - high affinity for O2 -
unaffected by pH, CO2 or BPG - binds 1 O2
2,3-bisphosphoglycerate
18
Myoglobin
- 153 Amino Acids - 77 Alpha-Helix - eight
Helices A, B, C, D , E , F , G , H - interior
residues are non-polar (Except His E7, His F8) -
exterior residues include both polar and
non-polar aa - contains a heme (haeme) cofactor -
porphyrin ring Fe2 Ion - required for protein
folding O2 Binding - O2 binds the Fe2 ion
19
Heme cofactor
Structure of heme, the cofactor in hemoglobin and
myoglobin
Figure 7.4
heme
20
O2 binding to heme
Heme binds O2 REVERSIBLY Gases like CO also
bind to heme BUT even more strongly than O2 -
explains why these molecules are highly
toxic What role does the protein (globin) portion
of myoglobin play? - it discourages the binding
of carbon monoxide, etc.
CO
CO
OO
Fe
Binding Pocket does not fit CO as well, but
binding is tighter
Fe
Binding Pocket fits O2 best
His
His
21
Coordination of iron by the protein and oxygen
His64
His93
Figure 7.5
22
Oxygen binding curve for myoglobin
A Hyperbolic Curve
Low P50 means high affinity
Figure 7.6
23
Figure 7.8 Binding curve required for an O2
transport protein Remember ? fraction of
binding sites occupied
Tissue lungs
High affinity at high O2 ? effective loading Low
Affinity at Low O2 ? effective unloading
24
Hemoglobin
- FOUR subunits
- - 2 alpha subunits (141 amino acids)
- - 2 beta subunits (146 amino acids)
- Each alpha and beta subunit individually looks
like myoglobin (However, only 24 aa conserved
among myoglobin, alpha and beta subunits) - - many different ways to get the same folding
normally need at least 15-25 aa identity between
proteins - Main Differences Between Hb and Mb are all due to
4 Str. for Hb - Cooperative Binding to O2
- Allosteric Regulation by CO2, H, and BPG (DPG)
tetramer
25
Hemoglobin Binds O2 Cooperatively
transition from weak to strong binding
Hemoglobin has a sigmoidal O2-binding curve this
type of curve is very efficient since it permits
full saturation of the protein in the lungs or
gills (high O2) and efficient O2 release in the
tissues (low O2). Such a binding curve reflects
weak versus strong binding, at low and high O2
pressures, respectively. This is due to the
existence of a cooperative or allosteric
interaction among the O2-binding sites in the
hemoglobin molecule i.e. the filling of the first
sites increases the affinity of the other sites
for O2. This phenomenon requires communication
between the different subunits regarding their
oxygenation state (filled or empty) it is only
possible because of the quaternary structure of
the protein.
myoglobin
PERCENT SATURATION
hemoglobin
OXYGEN PRESSURE
Strong binding- at high O2 pressures
weak binding- at low O2 pressures
Oxygen-binding curve for hemoglobin
26
Two models for the cooperative transition in
hemoglobin
Koshland-Nemethy-Filmer - a Sequential Model -
characterized by existence of some subunits in
weak some in strong states
Monod-Wyman-Changeux - a Concerted Model -entire
tetramer is in equilibrium between two forms
Figure 7.10
27
Structural changes of hemoglobinupon O2 Binding
- a significant change in the overall quaternary
structure of hemoglobin can be observed upon
oxygen binding. - rotation and sliding- brings b
chains closer together and narrows central
cavity -oxy state has higher O2 affinity- the
switch to this state is what causes cooperativity
in binding
Oxy-hemoglobin
Deoxy-hemoglobin
Figure 7.12
28
Heme causes the structural change
Figure 7.13
Binding of O2 causes a pull on helix F, resulting
in conformational changes throughout the protein
29
Experiment demonstrating the importance of the
movement of helix F
Figure 7.14
(a) Normal hemoglobin binding O2 - Cooperative O2
binding is observed - results in movement of F
helix (b) Mutant hemoglobin His ? Gly
mutation Free imidazole is then used to bind
heme This mutant hemoglobin still binds O2 but
without cooperativity
30
Other factors affecting the O2 affinity of
hemoglobin
- BPG (2,3-bisphosphoglycerate) lowers O2 affinity
of hemoglobin (not myoglobin). - Reduction in pH causes lower O2 affinity of
hemoglobin. - Release (accumulation) of CO2 in respiring
tissues lowers O2 affinity of hemoglobin.
31
BPG
Examining the affinity of hemoglobin in the
presence and absence of BPG demonstrates how
other factors can help modulate O2 binding - 1
molecule of BPG binds 1 tetramer - BPG is highly
charged (negative) and binds positively charged
side-chains and alpha - amino terminal groups
Binding site
32
Figure 7.18 Binding site of BPG
33
Effects of pH on O2 affinity of hemoglobin
- hemoglobin has reduced O2 binding at reduced pH
(acid) - this is useful affect because of reduced
pH in capillaries as a result of metabolic
products - having a lower pH at these areas where
O2 is to be delivered, increases the Transfer
Efficiency -molecular mechanism involves the
protonation of key histidines at lower pH
34
Fetal Hemoglobin
The predominant form of FETAL hemoglobin is
composed of 2 alpha chains 2 gamma
chains (i.e., gamma replaces beta) Fetal
hemoglobin has a HIGHER O2 affinity than adult
hemoglobin, but the affinity is still less than
that of myoglobin - allows for O2
transfer hemoglobin ? fetal hemoglobin ?
myoglobin - fetal hemoglobin also has a lower
affinity for BPG
35
Disease connected with hemoglobinsickle-cell
anemia
Results from a single mutation in the beta
chain Glu ? Val (-) charge is changed to a
nonpolar (hydrophobic) group This site of
mutation is at the surface of the protein in the
deoxy form of hemoglobin. ? This results in the
beta chains sticking together in the deoxy form
36
Sickle cell hemoglobin molecules
37
Sickle cell crisis
- low O2 causes a sickling crisis ? beta
chains form long fibers - these fibers distort
the shape of red blood cells - distorted RBCs get
jammed in capillaries and can clog them - RBCs
lyse ? anemia - capillary rich organs experience
impaired circulation ? organ damage
38
Sickle cell disease characteristics
39
Sickle cell anemia polymorphisms
- 1st genetic disease identified at a molecular
level - frequency high in areas where malaria is
a serious problem BALANCED POLYMORPHISM
Hb A Hb S Hb S Hb A Hb A Hb
S Malaria Relatively Sickle Cell (Death) Healthy
(Death)
40
Thalassemias
Diseases caused by mutations that either reduce
amount of hemoglobin chains or some chains are
absent ? one or more genes deleted ? nonsense
mutation may lead to truncated non-functional
protein ? mutation may affect gene expression
ß-Thalassemia ß-globin gene product
missing must rely on fetal ?-chains (usually
die in childhood) ?-Thalassemia ?-globin (2
genes- 4 copies) if 3 are defective see
health consequences - anemia if all 4 are
defective- can form only ?-chains- stillborn