CASE 1 - PowerPoint PPT Presentation
1 / 37
Title:
CASE 1
Description:
Colonoscopy in 1 y, repeat in 1 y if abnormal or at least every 2-3 y if negative for polyps. ... colonoscopy due to obstructing lesion, colonoscopy in ... – PowerPoint PPT presentation
Number of Views:77
Avg rating:3.0/5.0
Title: CASE 1
1
CASE 1
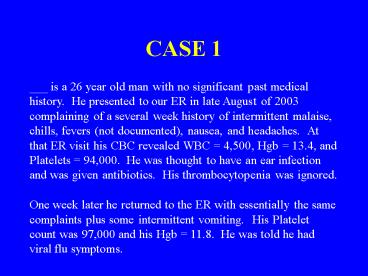
___ is a 26 year old man with no significant past
medical history. He presented to our ER in late
August of 2003 complaining of a several week
history of intermittent malaise, chills, fevers
(not documented), nausea, and headaches. At that
ER visit his CBC revealed WBC 4,500, Hgb
13.4, and Platelets 94,000. He was thought to
have an ear infection and was given antibiotics.
His thrombocytopenia was ignored. One week
later he returned to the ER with essentially the
same complaints plus some intermittent vomiting.
His Platelet count was 97,000 and his Hgb 11.8.
He was told he had viral flu symptoms.
2
Approximately 2 weeks later he returned to the ER
with the same complaints and was admitted for
further evaluations. At the time of admission,
he was afebrile and his physical examination was
essentially wnl. His CBC now revealed WBC
4,270, Hgb 8.9, and Platelets 123,000. What
do you do?
3
(No Transcript)
4
(No Transcript)
5
(No Transcript)
6
(No Transcript)
7
(No Transcript)
8
CASE 2
___ is a 62 year-old man who transferred his
medical care to the St. Louis VA Medical Center
in April of 2003. He came to the VA because he
needed medications for his diabetes and
hypertension. He gave a history of rectal cancer
so he was sent to our Hematology/Oncology section
for evaluation. We first saw him in May 2003.
His past medical history was somewhat complicated
information about his previous care was
obtained from the patient and his medical records
from several private physicians
9
Until August of 1996, ___ apparently enjoyed
excellent health and had no major chronic medical
problems except for cervical spondylosis
controlled with anti-inflammatory agents. His
past medical history was significant, however,
for a PE following knee surgery 20 years
earlier. His family history was unremarkable.
His problems began in late August of 1996 when he
presented to his physician complaining of 2 week
history of diarrhea and 7-10 day history of
fevers and chills. He also noticed a ?boil on
his right buttock. He saw his primary care
physician, was found to have a right perianal
abscess (ischiorectal abscess), and was
hospitalized. When he was seen by a surgeon, the
abscess was spontaneously draining.
10
The following day he was taken to surgery and
this large abscess was drained. His course was
complicated by a persistent leukocytosis (WBC
count 26-27,000). Because of this a rectal
exam was done, revealing a mass lesion on the
right side of the rectum. Biopsies established a
diagnosis of deeply invasive rectal
adenocarcinoma with moderate differentiation. He
underwent a diverting sigmoid colostomy and was
continued on antibiotics. His hospital course
was complicated by episodes of supraventricular
tachycardia and by a documented PE. At the time
of discharge in mid September of 1996 his abscess
was healing and his INR was therapeutic.
11
ANORECTAL ABSCESSES
The majority of anorectal abscesses and fistulas
originate from infected anal glands. Blockage of
anal glands permits the growth of bacteria, which
may ultimately lead to an abscess. Symptoms
almost always include pain although fever and
malaise are often present as well. Ischiorectal
abscesses penetrate through the external anal
sphincter into the ischiorectal space and present
as a diffuse, tender, indurated, fluctuant area
within the buttocks. They generally require
draining in the operating room where one can give
adequate anesthesia. Our patient was thought to
have developed an ischiorectal abscess due to
penetration of the rectal wall by an endophytic
carcinoma of the rectum. What other studies
should be considered?
12
(No Transcript)
13
Additional studies included CT scans of the
abdomen and pelvis were remarkable only for
showing the perirectal abscess. His CEA was
30.9. A rectal ultrasound examination was not
done. His physicians decided to treat his
abscess with antibiotics. Following treatment
and healing of his infection, his cancer was to
be treated. How should he be treated?
14
(No Transcript)
15
The patient responded extremely well to
antibiotics with healing of the abscess. In late
October of 1996 radiation therapy and 5-FU
chemotherapy was begun. He tolerated this
therapy well . Between 10/22/1996 and 11/25/96
he received 4500 cGy to his pelvis.
Subsequently, in early February of 1997, the
tumor was resected (APR). Pathology was
remarkable for only a small focus of microscopic
residual of adenocarcinoma but no evidence of
metastatic disease. The surgical margins were
clear and all 12 resected lymph nodes were
negative for metastatic disease. Following his
surgery, he received 4 cycles of adjuvant
chemotherapy (5-FU and Leucovorin). How should
he be followed now?
16
Surveillance after Colorectal Cancer
While intensive postoperative surveillance
programs have been justified in the hope that
early detection of asymptomatic recurrences will
increase the proportion of patients who are
potentially eligible for curative therapy, there
are few data to support a survival benefit from
such an approach. Its well recognized that
there is a subset of patients with 1. locally
recurrent or anastomotic disease, or 2. a limited
number of metastases involving liver or lung, or
3. metachronous (second primary) malignancies or
polyps who are potentially curable with further
surgery. In general, resection of a single
isolated site of metastatic disease results in
long-term relapse-free survival in approximately
20 to 25 percent of patients who are referred for
potentially curative surgery. However, this
subset of patients is small.
17
(No Transcript)
18
Surveillance
- History and physical every 3 mo for 2 y, then
every 6 mo for a total of 5 y - CEA every 3 mo for 2 y, then every 6 mo for y 2-5
for T2 or greater lesions - Colonoscopy in 1 y, repeat in 1 y if abnormal or
at least every 2-3 y if negative for polyps. If
no preoperative colonoscopy due to obstructing
lesion, colonoscopy in 3-6 mo.
19
During his first course of adjuvant chemotherapy
(in April of 1997), a repeat CEA was obtained.
His CEA 57. Now what do you do?
20
(No Transcript)
21
Because of his elevated CEA, CT scans of the
chest, abdomen, and pelvis were obtained. There
was no definite evidence of metastatic or
recurrent disease. He did have a presacral mass
but this was stable and was thought to be post
inflammatory. Now what do you do?
22
(No Transcript)
23
He was followed with serial CEAs which remained
in the 35-55 range. In addition, he had frequent
CT imaging of his chest, abdomen, and pelvis as
well as periodic colonoscopies. CT scans of his
abdomen and pelvis remained stable and without
evidence of recurrent/metastatic disease. In
August of 1998 CT scans of the chest showed a
small 1x1cm nodular density in the left lower
lobe posteriorly. This lesion was unchanged on a
follow-up CT scan studies done in April of 1999
and April of 2000. However, repeat CT scans of
the thorax done in May 2001 showed the soft
tissue nodule in the LLL had increased in size
and was now 2cm in diameter. A small area of
probable calcification was detected in the
nodule. Now what do you do? Surgery? PET
scan followed by surgery (if positive)?
Something else?
24
A PET scan was obtained in August of 2001 and was
entirely normal. Another CT scan study of the
thorax was obtained a year later in August of
2002. Now the soft tissue nodular mass in the
LLL had increased from 2.0cm to 2.8cm and the
lesion was spiculated. No other nodules were
identified and there was no lymphadenopathy. CT
scans of the abdomen and pelvis were stable and
essentially benign. A repeat PET scan was
obtained in September of 2002. This scan was
positive for the posterior left midlung mass
showing uptake of 18 FDG and consistent with
malignancy, either metastatic rectal cancer or
primary lung cancer (positive history for
smoking).
25
A biopsy was not done. Instead, the pulmonary
lesion was resected. In November of 2002 he
underwent a left posterolateral thoracotomy with
lower lobectomy. He tolerated this well without
complications. The pathology revealed a 3cm
metastatic, well differentiated adenocarcinoma
with mucinous features. Eight peribronchial
lymph nodes were negative for tumor. The tumor
was histologically similar to his prior rectal
carcinoma and immunostains supported a colorectal
origin and not a primary lung cancer. Now what
do you do?
26
(No Transcript)
27
- Postoperatively he continued to do well. In late
January of 2003 he again saw his oncologist. His
CEA was 60.2. He then transferred his care to
the St. Louis VA Medical Center, mainly so he
could obtain medications for his diabetes and
hypertension. - Now what do I do?
- Do nothing?
- Repeat the CEA?
- Repeat the scans?
- Another PET scan?
28
The CT scans were actually repeated by a VA
primary care physician before the patient was
sent to me. CT scans of chest, abdomen, and
pelvis were essentially unremarkable showing only
post-op changes including the presacral density
previously described since the time of his
initial presentation in 1996-1997. His CEA
100 A PET scan was ordered (to reinvent the
wheel).
29
(No Transcript)
30
A serum calcitonin was ordered. CALCITONIN,
SERUM RESULT 2970 PG/ML REF
highly suggestive of Medullary Thyroid Carcinoma
31
CT scans of the neck revealed an enlarged left
lobe of the thyroid gland 3.5x2 cm. A thyroid
scan demonstrated a large "cold" nodule in the
upper 2/3 of the left lobe of the thyroid gland
that also appeared to be enlarged compared to the
right lobe. Repeat PE showed at best a slight
fullness of the left thyroid gland without a
definite mass. FNA established the diagnosis of
Medullary Thyroid Carcinoma.
32
On November 25, 2003 the patient had a total
thyroidectomy, bilateral central neck dissection,
and parathryoid autotransplantation. Pathology
showed a tumor measuring Microscopic examination
showed medullary carcinoma involving the left
lobe with capsular invasion, but without
extension to soft tissues. All lymph nodes were
negative for tumor. Pathological Stage T2 N0 MX
(Stage II). Of note, there was no evidence in
any of the surgical specimen of C-cell
hyperplasia.
33
- MEDULLARY THYROID CARCINOMA
- A neuroendocrine tumor of the parafollicular or C
cells of the thyroid gland - Two forms 80 are sporadic 20 are familial
as part of the multiple endocrine neoplasia type
2 (MEN-2) syndrome - The most common presentation (sporadic) -
solitary thyroid nodule - In most patients, the disease is metastatic at
the time of diagnosis 50 have clinically
detectable cervical LN involvement although only
5 have evidence of distant disease at the time
of diagnosis
34
- MEDULLARY THYROID CARCINOMA
- The diagnosis is established by fna. Additional
staging includes biochemical and radiological
evaluations. - Measurements of serum calcitonin and CEA
- Evaluations for regional and distant metastases
with CT scans of the neck, chest, and upper
abdomen - Evaluations for MEN-2
35
MEDULLARY THYROID CARCINOMA Patients with
medullary thyroid carcinoma can be cured only by
complete resection of the thyroid tumor and any
local and regional metastases. Patients who
have normal serum CEA and serum calcitonin values
6 months after surgery are considered
biochemically cured and have the best prognosis
if biochemically cured, the 5-year recurrence
rate is only 5 and the overall survival rate is
98 at 10 years.
36
(No Transcript)
37
FINAL QUESTION What am I going to do if his
calcitonin doesnt fall to a normal level????