Deliberate SelfHarm: Definition - PowerPoint PPT Presentation
1 / 19
Title:
Deliberate SelfHarm: Definition
Description:
DSH is a compromise to avoid suicide (Walsh & Rosen, 1988) DSH differs from suicide only in clarity, intensity and expectation (Brown et al. ... – PowerPoint PPT presentation
Number of Views:217
Avg rating:3.0/5.0
Title: Deliberate SelfHarm: Definition
1
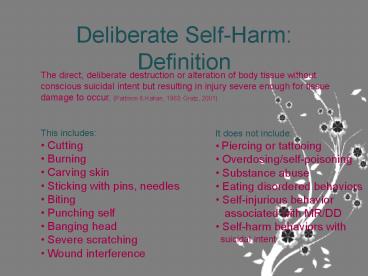
Deliberate Self-Harm Definition
The direct, deliberate destruction or alteration
of body tissue without conscious suicidal intent
but resulting in injury severe enough for tissue
damage to occur. (Pattison Kahan, 1983 Gratz,
2001).
- This includes
- Cutting
- Burning
- Carving skin
- Sticking with pins, needles
- Biting
- Punching self
- Banging head
- Severe scratching
- Wound interference
- It does not include
- Piercing or tattooing
- Overdosing/self-poisoning
- Substance abuse
- Eating disordered behaviors
- Self-injurious behavior
- associated with MR/DD
- Self-harm behaviors with
- suicidal intent
2
Terminology
- Deliberate self-harm is sometimes called
- Self-injurious behavior
- Non-suicidal self-injury
- Parasuicide
- Suicide gesture
- Self-mutilation
- We use deliberate self-harm because it is the
least pejorative and least stigmatizing of these
terms. It is also the term suggested in one of
the seminal papers in the field.
3
Favazzas Typology of Self-Mutilation (1988)
- Major Self-Mutilation
- Rare and typically seen in people with psychotic
disorders, mania or severe drug intoxication. - Includes severe self-mutilating behaviors such as
eye enucleation or amputation of limbs,or
self-castration. - Explanations given are usually based in religious
or sexual delusions, or delusions of sinfulness. - Identification with Christ
- Biblical or demonic influence
- Commands from God
- Desire to be female
- Control of sexuality
Favazza, 1988 Favazza, 1989, Favazza, 1998
4
Favazzas Typology of Self-Mutilation (1988)
- Stereotypic Self-Mutilation
- Common among individuals with mental retardation
and developmental disabilities (autism,
Lesch-Nyhan disease, Tourettes syndrom) - Includes behaviors such as scratching, biting,
head-banging, oral injuries (biting/picking of
lips, gums) - Hypotheses for this type of behavior
- Social reinforcement (behavior decreases in the
absence of adults) - Negative reinforcement (the behavior is used to
end an aversive situation, such as classroom
time) - Self-stimulation in the absence of adequate
neurosensory stimulation, an individual will
engage in self-harming behavior to stimulate
himself (also found in normal-intelligence
infants and animals).
5
Favazzas Typology of Self-Mutilation (1988)
- Moderate/Superficial Self-Mutilation
- Most commonly seen in women, with onset in
adolescence - Most common form is skin cutting, though 75 use
multiple methods - Numerous, wide-ranging explanations for the
behavior - Tension release
- Anti-dissociation
- Interpersonal control/influence
- Social functions (identity formation, group
membership)
6
Prevalence
- Community Samples
- Adolescents 13-16 (Ross Heath, 2002
Muehlenkamp Gutierrez, 2004) - College Students 17-36 (Gratz, 2001 Whitlock
et al. 2006 Brown et al. 2007) - Adults 4 (Klonsky, et al., 2003 Briere
Gil, 1998) - Clinical Samples
- Inpatient adolescent 24-82 (Taimenin et al.
1998 Rosen Walsh, 1989 Nock Prinstein,
2004) - Inpatient adult 21-35 (Briere Gil, 1998
Paul et al. 2002) - Inpatient BPD 75-80 (Soloff, 1994 Shearer et
al., 1988)
7
Who Self-Harms?
- Men and women engage in the practice equally,
though women are more likely to seek treatment. - Most people begin in adolescence or in their
early twenties, and the behavior tends to
decrease in the 40s and 50s. - Those who start earlier are somewhat more severe
and DSH may be more persistent - No association with race or SES
- LGBT have a higher rates of DSH
8
Risk Factors
- The most consistent risk factor for DSH is
childhood abuse-- physical, sexual, emotional
abuse and neglect. - For men only, childhood separation from the
father is a risk-factor - Familial alcohol abuse
- Dissociation
9
Deliberate Self-Harm and Suicide
- Although some clinicians and researchers put DSH
on a continuum with suicide - both acts embrace a self-destructive drive
towards death (Suyemoto, 1998) - DSH is a compromise to avoid suicide (Walsh
Rosen, 1988) - DSH differs from suicide only in clarity,
intensity and expectation (Brown et al. 2002
Linehan, 1993). - Most self-harmers describe DSH as distinct from
suicide both in intent and the emotional
processes involved. - However, many individuals who self-harm also
report suicide ideation or suicide attempts. - In clinical and community samples of adolescents
and young adults, 28-39 of those with
moderate-severe or repeated DSH reported suicidal
ideation, plans, or attempts. (Lloyd-Richardson
et al. 2007 Walsh Rosen, 1988 Whitlock et al.
2006)
10
Deliberate Self-Harm and Suicide
- Different Reasons for Suicide Attempts and DSH
(Brown et al. 2002) - DSH Feeling generation, self-punishment, anger
expression, distraction (among other reasons) - Suicide attempt to make others better off (among
other reasons) - Evidence of different emotional processes
(Chapman Dixon-Gordon, 2007) - DSH relief was the most common emotional
consequence - DSH associated with a positive shift in emotions
69 of the time - Suicide attempt Anger and guilt were the most
common emotional antecedents and the most common
emotional consequences. - Other researchers have suggested that the
difference between suicide and DSH is that those
who commit suicide experience before the suicidal
act, and those who self-harm experience relief
afterward (Walsh Rosen, 1988) - DSH could be anti-suicide
- DSH alleviates dissociated, depersonalized,
deadened states and therefore moves the
self-harmer toward feeling more alive.
11
Functions of Deliberate Self-Harm
- One of the most difficult tasks in attempting to
understand any pathological behavior is
discerning why this particular behavior at this
particular time to serve this particular function
for this particular patient (Suyemoto, 1998,
537). - In understanding deliberate self-harm, the task
is to understand the functional aspects of the
behavior.
12
Related Diagnoses
- In the DSM-IV, DSH is only listed as criteria for
BPD but it is commonly seen in several other
clinical populations. - Borderline Personality Disorder 75-80
(Herpertz, 1995) - Eating disorders 40-85 of ED patients (Claes,
Vandereycken Vertommen, 2001, 2003 Paul et al.
2004 Linehan et al. 2006 Herpertz, 1995) - Depression 35-96 (Kumar et al. 2004 Briere
Gil Matsumoto, 2004, Soloff, 1994 Linehan et
al. 2006) - Substance abuse 25-30 (Briere Gil, Matsumoto,
2004 Linehan et al. 2006) - Posttraumatic Stress Disorder 50 (Matsumoto,
2004 Linehan, 2006) - Any psychiatric comorbidity 41-87 (McAuliffe et
al. 2001 Lloyd-Richardson et al. 2007 Kumar et
al. 2004)
13
DSH in BPD
- DSH has been called the behavioral specialty of
BPD occurs in 75-80 of those with BPD (Gratz
Gunderson, 2006) - Emotion regulation function The hallmark of BPD
is emotional distress (chronic feelings of
hopelessness, depression, anger, anxiety),
coupled with ineffective attempts to regulate
emotions. - Interpersonal influence?
14
Nock and Prinsteins Function Subscales
- Automatic-Negative Reinforcement
- Relief from aversive internal states makes the
behavior more likely - To stop bad feelings to relieve dissociated
states - Automatic-Positive Reinforcement
- A desirable internal consequence makes the
behavior more likely - To feel something, even pain to punish yourself
to feel relaxed - Social-Negative Reinforcement
- Relief from a negative external experience makes
the behavior more likely - To get out of something you dont want to do to
avoid punishment to avoid other people - Social-Positive Reinforcement
- A desirable social/external consequence makes the
behavior more likely - To get control of a situation to get a reaction
from others to give yourself something to do
when youre alone to get attention -
- (Nock Prinstein, 2004)
15
Emotion Regulation Model of DSH(automatic-negativ
e reinforcement)
- 96 of self-harmers (with BPD) reported that
emotion release was the reason for the behavior.
(Brown et al. 2002) - Emotional dysregulation develops through a
combination of individual risk factors (emotional
reactivity and intensity) and environmental risk
factors (invalidating environments that fail to
teach strategies for emotion regulation. - DSH may develop as a way to manage intense or
out-of-control emotions. It may serve to - Reduce anxiety - Release tension
- Release anger - Provide a sense of control
- Relieve guilt, loneliness - Concretize
emotional pain - Terminate dissociation - Stop racing thoughts
- Gratz, 2003 Briere Gil, 1998 Connors,
1996 Linehan, 1993
16
Chapman, Gratz Browns Experiential Avoidance
Model
- Experiential avoidance any effort to avoid or
escape internal experiences or the situations
that produce them - Experiences thoughts, feelings or physical
sensations - Avoidance strategies thought suppression,
avoidance substance abuse, DSH. - Avoidance is negatively reinforced since, when
you avoid, immediate discomfort is reduced. This
relationship becomes very strong after repeated
experiences.
17
Chapman, Gratz Browns Experiential Avoidance
Model
- In the long term, thought suppression tends to
increase distress, increase the frequency of
distressing thoughts and increase the likelihood
of a rebound effect from the suppressed emotional
experience (ie temporary relief leads to greater
anxiety) - Avoidance decreases the likelihood of extinction
of unwanted emotions and prevents the individual
from learning that aversive emotional states,
while unpleasant, are not threatening.
18
Interpersonal Functions?
- Often clinicians, family members and friends of
self-harmers are influenced by the behavior so
they assume that the self-harmers intent is
manipulation or control. (Linehan, 1993 Favazza,
1989 Gratz, 2003). - There is some evidence of interpersonal an
expressive functions of self-harm (Nock
Prinstein, 2004 Favazza, 1989), and also that
the interpersonal functions might be an
unintended consequence or secondary to the
emotion regulation functions. - In studies of DSH, interpersonal influence is
never given as the primary reason for the
behavior. - However, there seems to be another subset of
self-harmers who never disclose that they engage
in the behavior. - 35 of self-harmers reported that they never
told anyone about it (Whitlock, 2006)
19
Empirically Supported Treatment
- Emotion-Regulation Group Treatment Gratz
- 14-week emotion-regulation group therapy (added
to other therapies). - Draws on DBT and Acceptance and Commitment
Therapy, with emphasis on - Identification of functions of DSH
- Emotional clarity and awareness, functions of
emotions - Benefits and consequences of emotional acceptance
(ie that non-acceptance may amplify negative
emotions) pain vs suffering - Identifies valued directions and commitment to
valued actions - Treatment participants showed significant
decreases in DSH, depression, emotional
dysregulation, stress and anxiety.



























![[DOWNLOAD] Duty to Deliberate: Justice by Chance or by Design? Kindle Edition PowerPoint PPT Presentation](https://s3.amazonaws.com/images.powershow.com/10058865.th0.jpg?_=20240619094)


![[PDF] DOWNLOAD Three Invaders: The Deliberate Revision of Hi PowerPoint PPT Presentation](https://s3.amazonaws.com/images.powershow.com/10119341.th0.jpg?_=202409030912)