Adrenergic Drugs 1 receptor - PowerPoint PPT Presentation
1 / 54
Title:
Adrenergic Drugs 1 receptor
Description:
Some vascular smooth muscle. Inhibition of transmitter release ... Phentermine (lonamin, phen-phen) (C-III) Narcolepsy: Dextroamphetamine (Dexedrine) ... – PowerPoint PPT presentation
Number of Views:3011
Avg rating:3.0/5.0
Title: Adrenergic Drugs 1 receptor
1
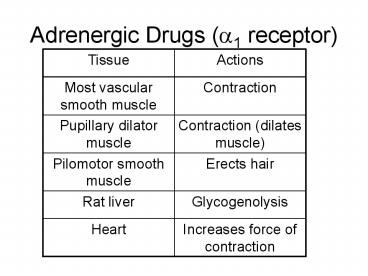
Adrenergic Drugs (?1 receptor)
2
Adrenergic drugs (?2 receptor)
3
Adrenergic drugs (??1 receptor)
4
Adrenergic drugs (?2 receptors)
5
Adrenergic drugs (?3 receptors)
6
Adrenergic drugs (D1 receptors)
7
Adrenergic drugs (D2 receptors)
8
Adrenergic drugs receptor affinities
9
- DA can interact with alpha or beta receptors,
especially at higher concentrations. - There are specific DA receptors also DA
receptors are especially important in the CNS and
in renal vasculature - Alpha-1 receptors are post-synaptic and mainly in
smooth muscle. - Alpha-2 receptors are mainly pre-synaptic located
at nerve terminals in the CNS they may be
located on post-synaptic membranes as well. - The molecular mechanisms of both alpha and beta
receptors involve interaction of a catecholamine
with the receptor coupled to a G protein.
10
- Beta receptors activation of adenylyl cyclase
(AC) and increased synthesis of cAMP via a
stimulatory Gs protein. cAMP serves as a second
messenger leading to specific tissue changes via
activation of a cAMP dependent protein kinase. - ?1 receptors Activates phosholipase C (PLC) and
leads to release of inositol-1,4,5-triphosphate
(IP3) and diacylglycerol (DAG) via Gq protein. - ?2 receptors Inhibition of AC and decreased
intracellular levels of cAMP via an inhibitory GI
protein. - D1 receptors Stimulates an AC.
- D2 receptors Inhibits AC and opens K channels.
11
- Desensitization/down - regulation--tolerance,
tachyphylaxis (rapid appearance of progressive
decrease in response following repetitive
administration of a pharmacologically active
substance), or refractionaries may develop with
exposure to catecholamines and other
sympathomimetics. Various mechanisms have been
invoked including phosphorylation or
internalization of receptors and decrease in
number of functional receptors. - Up-regulation/super-sensitivity--an increase in
the number of functional receptors.
12
- Pharmacokinetics
- Catecholamines are quite susceptible to monoamine
oxidase (MAO) and catechol-O-methyltransferase
(COMT) enzymes (liver, GI tract and many tissues
of the body) ineffective orally. - Rapidly taken up by active transport process in
sympathetic post-ganglionic nerve terminals and
other chromafin tissues--inactivated. - Metabolites (e.g. vanillymandelic acid - VMA) and
free amine excreted in urine.
13
- Pharmacodynamics Effects on Organ Systems
- Resemble the effects of sympathetic stimulation,
with some important differences the net effect
depends upon the relative receptor affinity,
intrinsic activity, and compensatory reflexes
evoked by the direct action of the drug. - Note EPI is usually given as a bolus injection
which causes it to stimulate the ?1 receptor in
skeletal muscle and skin causing
vaso-constriction same effect as NE. - PHE is a selective ? agonist.
- ISO is a selective ? agonist, it does not
stimulate the ? receptor. - NE can stimulate the ?1 receptor in the heart but
the effect is small when compared to the
baroreceptor reflex. - ISO will also set off the baroreceptor reflex but
opposite to that of EPI BOTH INDIRECT AND
DIRECT INFLUENCES ARE IN THE SAME DIRECTION.
14
CV Response to Sympathomimetic Amines
15
CV Response to Symapathomimetic Amines
16
CV Response to Sympathomimetic Amines
17
CV Response to Sympathomimetic Amines
18
CV Response to Sympathomimetic Amines
19
- Notes on CV response to sympathomimetic amines
- Since skeletal muscle has more blood volume than
skin effects on its receptors have a greater
effect on TPR. - TPR (SV)(CO)
- MABP (TPR)(CO)
- CO (HR)(SV), stroke volume is measured out of
the left ventricle. - When BP ? you set off a baroreceptor reflex which
? sympathetic outflow ? contractility. - Skin and splanchnic vessels have more ?1 than ?2
- Skeletal muscle has more ?2 than ?1.
20
- Notes on CV response to sympathomimetic amines
- NE is essentially a pure vaso-constrictor.
- Isoproterenol is essentially a pure vaso-dilator.
- EPI has mixed effects (? ?) depending on its
dose and site---can dilate blood vessels in
skeletal muscles (?2). - TPR increases with NE, decreases with
isoproterenol, and usually decreases with EPI. - Blood Pressure EPI and NE usually increase the
mean arterial pressure (MABP), although EPI can
lower diastolic pressure. - Isoproterenol usually decreases MABP, although
systolic pressure may rise.
21
- CV response to sympathomimetic amines
- All 3 drugs have cardiac stimulant properties.
- Rate and force of conraction are DIRECT EFFECTS.
- Any rise in BP however, elicits REFLEX SLOWING of
the heart (NE sometimes EPI), this is an INDIRECT
EFFECT. - Cardiac output INCREASED by EPI and
isoproterenol. - Cardiac output is unchanged or decreased with NE
due to vaso-constriction and indirect effects. - Conduction ? A-V conduction.
- DA activates several D1 receptors in several
vascular beds, which leads to vaso-dilation. It
also activates ?1 receptors in the heart. - At low doses, peripheral resistance may decrease.
At higher rates of infusion, DA activates
vascular ?1 leading to vaso-constriciton,
including the renal vascular bed.
22
- CV response to sympathomimetic amines
- ?2 stimulation generally results in relaxation
e.g. bronchioles, detrusor muscle of the bladder,
uterus and GI tract. - Alpha receptors ?1 receptor mediates
contractions e.g. radial smooth muscle of the
iris (mydriasis), sphincters of the bladder and
GI tract. - Alpha-agonists that stimulate ?2 receptors
promote relaxation of GI smmoth muscle indirectly
by pre-synaptically reducing the release of
acetylcholine (its an auto-receptor that acts by
a pre-synaptic mechanism).
23
- Sympathomimetic amines metabolic and endocrine
effects - EPI (and to a lesser extent NE and ISO) elevates
concentrations of glucose in the blood mediated
primarily by ?2 receptors. There is ?
glycogenolysis and gluconeogenesis due to
stimulation of the beta receptor. - Insulin is inhibited by ?2 receptors and enhanced
by ?2 receptors the predominant effect with EPI
is inhibition with ISO its stimulation. - Catecholamines raise blood free fatty acid levels
by stimulating ?3 receptors in adipocytes. - ?1 receptors stimulate renin secretion ??
angiotensin II which in turn increases BP.
24
- Sympathomimetic amines CNS
- Catecholamines can elicit mild CNS
stimulation--due indirectly to peripheral
effects cannot get into the CNS. - Miscellaneous these drugs facilitate
neuromuscular transmission in skeletal muscle and
beta adrenergic effects may promote tremor (?2) - Lower intra-occular pressure (IOP)--EPI--?1--this
is a paradoxical effect ? antagonist and ?
agonist can be used for tx of glaucoma by ?
diameter of blood vessels in the eye, ? aqueous
humor formation.
25
- Adverse reactions to sympathomimetic amines
- Mainly an ext of pharmacological prop, esp
pronounced on the heart. - Anxiety, forceful heart beat, palpitations, HA,
cardiac arrhythmias. - NE---tissue necrosis, sloughing.
- ISO---tremor, sweating, pallor.
- OD TOX LIFE THREATENING increases in BP,
cerebral hemorrhage (EPI NE) and angina
serious cardiac arrhythmias---esp vent
tachyarrhyth. - TX PROPRANOLOL PHENTOLAMINE (AGONIST).
26
- Sympathomimetic amines clinical uses
- CV applications hypotn states and shock
- Cardiogenic shock DA and ISO
- Topical hemostatic EPI---given by SC injxn _at_
high doses causing vaso-con to ? blood loss (used
in surgery). - EPI used in conjxn w local anesth to ?? systemic
absorp, prolong action (1 200,000) - Anaphylaxis EPI remains the ER DOC for
anaphylactic shock---physiologic antagonist
(bronchial dilator).
27
Sympathomimetics clinical uses
- Bronchial asthma EPI and ISO replaced by
selective ?2 agonists (e.g. terbutaline) - Ophthalmic use EPI for glaucoma.
28
- Other sympathomimetics
- Ephedrine 1st orally active sympathomimetic
introduced from the herb ma-huang by K.K. Wang - MOA indirect - release of catecholammines from
storage sites in sympathetic N term some direct
effect on ? and ? adrenergic receptors-----tachyph
ylaxis can occur, acute tolerance develops
rapidly due to depletion of NE. - Pharm efx resemble those of EPI except
effective orally, ? duration of action, more CNS
stimulant properties and 4.) much lower potency
(bc does not have the catechol group) - Clinical uses sub for EPI, nasal decong, hypotn
and asthma.
29
- Adverse reactions with ephedrine
- CV CNS effects abuse because its available in
an herbal tea the FDA says that there is not
enough evidence or rationale to take ephedra off
the market. - It acts as a nasal decongestant by contracting
the nasal blood vessels that have been dilated
due to histamine. Most nasal decongestants are ?
agonists so they do not stimulate the heart
because it has ? rceptors.
30
- Amphetamine (?-phenylisopropylamine)
- MOA Indirect--release NE
- Pharmacological effects
- Similar to ephedrine EXCEPT more potent CNS
stimulant properties euphorigenic effects. - The d isomer (i.e. dextroamphetamine--speed) is
the most potent CNS stimulant whereas the L
isomer has slightly greater peripheral effects.
Methamphetamine enters the CNS even more readily
(i.e. ice, ecstasy, MDMA) - Clinical uses
- Short term use as appetite suppressant in
conjunction with appropriate diet exercise
efficacy diminishes with continued use. No
evidence that long-term improvement in weight
control can be achieved with amphetamines alone
anorexic effect.
31
- Amphetamine Clinical Uses
- diet pills w sim prop, degrees of abuse
potential - e.g. methamphetamine (Desoxyn) (C-II)
- Phentermine (lonamin, phen-phen) (C-III)
- Narcolepsy
- Dextroamphetamine (Dexedrine)
- Methylphenidate (Ratalin)
- Drugs work by ? alertness and ? sleep
- Attention deficit disorder (ADHD) in children
- Amphetamines (i.e. dextroamphetamine
methamphetamine, methylphenidate) paradoxical
effect--improved attention span with poss
improving learning--very strong ? effect in brain
may lead to vaso-con, decrease blood flow. - New form longer acting, 1/ day as opposed to 3-4
X day.
32
- Amphetamines Adverse Reactions
- Palpitation, angina, arrhythmias can cause death.
- Acute tox efx sympathomimetic efx, esp CV efx,
CNS stim--restlessness, insomnia, irritability,
confusion, anxiety, delerium. Poss convulsions,
coma, CVA, ? libido. - Chronic intoxication also includes psychotic
reactions--paranoid shizophrenia, with possible
hallucinations and suicidal or homicidal
tendencies. Additional toxicities (e.g.
pulmonary hypertension damage to heart valves)
were subsequently identified with fenfluramine
and dexfenfluramine, they were removed from the
market in 1997--violence and aggression.
33
- Other sympathomimetic agents with predominantly
vasoconstrictor (?) activity - Phenylephrine (NeoOSynephrine)-pure ? agonist
- Phenylpropanolamine
- Imidazole derivatives (naphazoline)--mainly used
as a vasoconstrictor nasal decongectant
hypotension as a result of shock. - Principle vasocon (nasal decong hypoTN states)
- Phenylephrine is also used as a mydriatic.
- Phenylephrine - direcct acting ?1 selective
agonist. - Phenylpropanolamine--related to ephedrine and
amphetamine used as a nasal decongestant---warnin
g--CV toxicity in high doses. - NOTE selective ? 2 adrenergic agonists (e.g.
clondine) mainly used for HTN.
34
- BETA RECEPTOR SELECTIVE AGONISTS
- ?1 selective agonists Dobutamine--a syntheitc
catecholamine related to DA. It has relative
slectivity for ?1 receptors and used in acute
heart failure and cardiogenic shock. - ?2 selective agonists
- Terbutaline
- Albuterol
- All are only relatively slective for ?2
receptors. - Principle uses are as bronchodilators and to
delay premature labor (ritodrine, terbutaline) by
relaxing the uterus.
35
- ADRENERGIC BLOCKING AGENTS ADRENOCEPTOR
ANTAGONIST - The classical alpha - adrenergic blocking
agents (?1, ?2) include - Ergot alkaloids---first discovered in 1905
variable effects and many side-effects (e.g.
ergotamine) - Phentolamine (Regitine)---competitive, reversible
antagonists--non-selective. - Phenoxybenzamine (Dibenzyline)---potent,
irreversible blocking agent---non-selective. - Relatively selective alpha receptor blocking
agents - Prazosin (Minipress) HTN
- Yohimbine (Yohimex) Impotence, ?2 receptor.
36
- Adrenoceptor antagonists Pharmacologic effects
- Prevent sympathetically mediated excitatory
responses at smooth muscle exocrine glands. - Net effects depend on dosage (i.e. dose
dependent), degree of sympathoadrenal activity,
circulating amine levels, as well as relative
degree of slectivity. - CV effects
- Blood vessels
- vaso-dilation IF sympathetic tone is high (in
HTN) - Interfere with compensatory (baroreceptor)
reflexes ? postural reflex--causes fainting and
syncope. - Block vaso-constrictor action of
symopathomimetics.
37
- Adrenoceptor pharmacologic effects
- Blood pressure
- Decreased
- Block increase in BP caused by sympathomimetics
- Epinephrine reversal--converts an oppressor
response to a depressor response. - Heart
- Minimal direct effects
- Tachycardia if BP fails---reflex
- Other effects
- Miosis
- Nasal stuffiness by blocking ? receptor in the
sinuses
38
- Adrenoceptor adverse reactions
- Adverse reactions
- Phentolamine----reflex cardiac stimulation due
to enhanced NE release (via ?2 blockade) possess
parasympathomimetic and histamine like effects
as well tachycardia, cardiac arrhythmias,
anginal pain, NVD, exacerbation of peptic ulcer,
hypotension (orthostatic) - Phenoxybenzamine----postural hypotension, reflex
tachycardia, nasal congestion, miosis, inhibition
of ejaculation, sedation, nausea, weakness and
local tissue irritation.
39
- Adrenoceptor clinical uses
- Pheochromocytoma---
- CA of the adrenal medulla ? release of
catecholamines (NE) - HTN and tachycardia - Pre-operative management ? HTN
- Local vaso-con XS----phentolamine, or frostbite,
? blood supply to the region - Periph vasc dz--ltd.---Raynauds dz Ca2 channel
blockers also effective for tx. - Genitourinary---phenoxybenzamine (Dibenzyline)
prostatic hypertrophy (e.g. BPH relaxes muscle at
base of prostrate), plastocyn also - Phentolamine papaverine for impotence---injxn
inconvenient---replaced by Viagra. - Note selective alpha 1 blocking agents are
effective anti-hyperTN agents w less tachycardia
side-effects.
40
- Beta - receptor antagonists
- Numerous beta receptor blocking agents have been
developed - Non-selective
- Propranolol
- Nadolol
- Timolol
- Pindolol
- Sotalol
- ?1 selective cardioselective
- Metoprolol
- Acebutolol
- Atenolol
- Esmmolol
41
Beta receptor antagonists
- Beta receptor blocking drugs with partial
agonistic activity intrinsic sympathomimetic
activity (ISA) - Pindolol
- Acebutolol
42
Properties of beta receptor blocking drugs
43
Properties of beta receptor blocking drugs
44
- Pharmocokinetics of beta receptor blocking agents
- Absorption
- Well absorb after oral admin bioavail varies
widely (e.g. propranolol exten 1st pass metab
consequences---ONLY 30 IS BIOAVAILBLE) - Indiv varia after oral admin--must titrate dose
individually. - Distribution and elimination
- Rapidly distributed some do not readily enter
CNS (e.g. nadolol atenolol) H2O soluble. - Most 1/2 lives are approximately 3-6 h
exceptions-- - Esmolol is shortest (10 minutes) used in the ER
for cardiac arrhythmia - Nadolol is longest (up to 24 h)
45
- Pharmacokinetics of beta receptor blocking agents
- Distribution and elimination
- Degree of biotransformation varies considerably
- Propranolol, metoprolol and timolol are
extensively metabolized in the liver. - Pinolol and atenolol are less completely
metabolized - Nadolol is excreted unchanged in the
urine--therefore dose must be adjusted for renal
problems - Esmolol is an ester and is rapidly metabolized by
esterases in RBCs.
46
- Beta receptor blocking agents pharmacodynamics
- Non-selective beta receptor blocking agents block
sympathetically mediated - Cardiac acceleration-chronotropy (?1)
- Increased myocardial contractility-inotropy (?1)
- Vaso-dilation (?2)
- Bronchiolar dilation (?2)
- Hyperglycemia (?2)
- Cardioselective beta blockers show more selective
block of cardiac (?1) effects at lower doses
higher doses come with other effects as well. - Cardiac effects
- ? HR, contractility, ? SV and ? CO ?BP
- ? A-V conductiondromotropy---a dromotropic
effect deals with A-V conduction.
47
- Beta receptor blocking agents pharmacodynamics
- Blood pressure
- With increased P-R interval--contr to
anti-arrhythmia effect - Mechanisms of BP lowering
- Block the release of renin (?1 mediated)
- ? CO and TPR (?1 med), either no change or
increased because there is no effect on ?
receptors. - CNS effects
- ? ?2 receptor ? ? sympathetic outflow.
- Eye
- ? IOP---paradoxical (? aqueous humor formation)
- Other effects
- Bronchioles constrict thus exacerbate asthma
COPD - Metab efx ? glycogenolysis, ? glucagon, ?
lipolysis hypoglycemia - Partial agonists pindolol and acebutolol
- CNS stim/depress (only w drugs w hi lipid
solub) drowsiness, fatigue and sedation.
48
- Beta receptor blocking agents adverse reactions
- Extensions of the pharmacological effect
- CV ?1
- Bradycardia
- CHF
- Hypotension
- A-V block
- Bronchioles ?2
- Asthma wheezing
- Bronchospasm
- Other
- GI----NVD
- CNS
- allergic
49
- Beta receptor blocking agents clinical uses
- HTN
- Angina pectoris
- Tx acute MI and prevent recurrent MI, by
decrease work of myocardium. - Cardiac arrhythmias
- Hypertrophic sub-aortic stenosis---cardiomyopathy
- Glaucoma--topical (e.g. timolol)
- Hyperthyroidism
- Migraine---propranolol---prophylaxis
- Reduce anxiety---? stage fright
50
Beta receptor blocking agents contra cxn
- CHF
- Cardiogenic shock
- A-V block
- Sinus bradycardia
- Asthma
- Diabetes
- DO NOT DISCONTINUE ABRUPTLY WHEN TREATING ANGINA
51
- Mixed aplha and beta blocking drugs
- Labetalol
- Non-selective beta-receptor blockade tends to
predominate, but at higher doses, both alpha and
beta blocking effects result. It is an effective
anti-HTN drug produces a fall in BP with less
tahycardia than occurs with phentolamine.
Orrally effective. - Carvedilol
- Has anti-HTN activity and is useful adjunctively
in certain types of congestive heart failure.
52
- Other sympathoplegic drugs anti-HTN agents
- There are numerous sites at which drugs may act
to alter sympathetic nervous system function and
weaken adrenergic influences - Adrenoceptors on effector cells innervated by
sympathetic post-ganglionic fibers--i.e.
adrenergic blocking agents. - Sympathetic post-ganglionnic nerve terminals
- Symapthetic ganglia
- CNS
53
- Adrenergc neuron blocking agents
- Adrenergic neuron blocking agents drugs that act
on post-gang symp N terminals to interfere w norm
physio release of NE - Guanethidine---displaces NE from vesicles and
depletes stores and also blocks the physiologic
release of NE. - Consequences chemical sympathectomy
- Transient initial sympathomimetic effect (IV)
- Generalized sympathetic nervous system depression
- Supersensitivity of effector cells to
catecholamines - Uses severe HTN--very little use now due to
serious side effects and drug interactions. - Reserpine
- MOA impairs storage of catecholamines in
adrenergic N term drug is metab by MAO - Used for mild HTN.
54
Centrally acting sympathoplegic drugs
- Methyldopa
- MOA decreases BP by reducing peripheral
vascular resistance and a variable reduction in
both heart rate and cardiac output. - Clonidine
- ?2 agonist.