Caithness Geography - PowerPoint PPT Presentation
1 / 24
Title:
Caithness Geography
Description:
... addressing quality issues and a spur to the development of more adequate data ... To be effective clinical governance will require data about the quality of care. ... – PowerPoint PPT presentation
Number of Views:33
Avg rating:3.0/5.0
Title: Caithness Geography
1
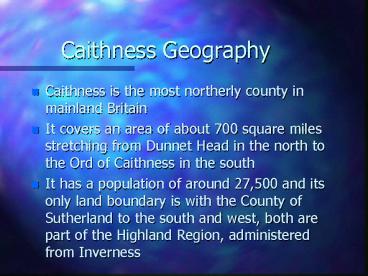
Caithness Geography
- Caithness is the most northerly county in
mainland Britain - It covers an area of about 700 square miles
stretching from Dunnet Head in the north to the
Ord of Caithness in the south - It has a population of around 27,500 and its only
land boundary is with the County of Sutherland to
the south and west, both are part of the Highland
Region, administered from Inverness
2
Caithness Geography
- The two main towns in Caithness are Wick, with a
population of around 8,000, once famous as the
herring capital of the world and Thurso,
population around 12,000, with close ties to the
U.K.A.E.A. site at Dounreay
3
Caithness Community Mental Health
TeamOperational policy (under amendment)
- The Community Mental Health Team (CMHT) is based
at Community Mental Health Services, Bankhead
Road, Wick. - The team currently works from 9am -5pm Monday -
Friday. - There is currently no out of hours service within
the CMHT. Mental health officers are accessed
through Area Social Work team, or social work
standby - Currently looking at expanding hours
4
Core Statement
- The CMHT is funded with mental health resource
transfer monies and Primary Care Trust funding to
enable comprehensive mental health services to be
provided in the Caithness community and will work
collaboratively with the Local Health Care
Co-operative (LHCC)
5
Core Statement continued
- Service to those who experience severe and/or
enduring mental illness are prioritised. - Time limited intervention to those who experience
mild to moderate problems are provided but may
have a delay in response time
6
Service Elements
- The community team has 3 service
elements(a) Substance misuse service
(CMHN)(b) Older Adult service (CMHNs)(c) Multidi
sciplinary Generic Team (MDT)All interact with
each other although each service has a different
focus
7
Team Members
- Community Mental Health Nurses
- Social Workers
- Technical Instructor
- Accommodation Support Officer
- Group Worker
- Consultant Psychiatrist
- Support Workers
- Team Leader
- Clerical Staff
8
Team Members (continued)
- A clinical psychologist holds clinics in both
Wick and Thurso, on a monthly basis, and provides
consultation to CMHT members. - Various interventions are offered by the team
depending on the individuals clinical need.
These are offered on a 1-1, 2-1 or group basis.
9
Referrals
- All adults aged from 16-65 years who experience
mental ill health can be referred to the
Community Team - Referrals are received by letter through the team
manager. Urgent referrals may be telephoned to
either the team manager or, in her/his absence,
the professional on duty with the letter to
follow.
10
Referrals
- Referrals are considered at the weekly team
meeting where allocation for initial assessment
is completed - Primary addiction problems would be referred
directly to substance misuse nurse. - Persons aged over 65 years with either functional
or organic illness will be assessed by one of the
older adult CMHNs and referrals made direct to
them.
11
Do We Use Outcome Measures?
NO
12
AVON Mental Health MeasurePositive Aspects
- 3 Statements surrounding
- ease of use of AVON measure
- usefulness of AVON measure in identifying areas
of need - participants motivation in changing identified
areas of need
13
AVON Mental Health MeasurePositive Aspects
continued
- Provides information to better plan services
- Allows client to build up a profile about
themselves - Service users are central to individual needs
assessment, enhancing their role will improve
both process and outcome
14
AVON Mental Health MeasurePositive Aspects
- Identifies unmet needs, thus a method for
recording gaps in services etc. - From Staff perspective - forum for discussion -
increase understanding of clients difficulties
15
AVON - User Mental Health Assessment Measure
- Undertook small presentation to CMHT - HONOS
AVON - Team Decided to look more closely at AVON measure
- Rating scale devised and sent out to participants
- Statements devised using the Likert rating scale
16
RESULTS of Questionnaire
- AVON TOOL identified as easy to use
- AVON tool useful in identifying areas of need
- However, clients identified difficulty with
motivating themselves to make changes
17
AVON Results
18
AVON Results
19
AVON Results
20
Evaluation of questionnaire (AVON)
- Overall the AVON measure identified wider issue
gaps - Central theme of unmet needs consistently
appeared to surround stigma and discrimination - Users found the tool easy to use
- Identifying area of need was useful, I.e.
increasing understanding, insight into
difficulties - Motivating clients to make change in areas
slightly more difficult - Identified by Whitehead-Black report
21
CONCLUSION
- This project has highlighted issues for the
Caithness Community Mental Health Team,
surrounding the ethos of what we are attempting
to strive towards with clients. - There remains a great deal of work and innovation
to changing community/public perceptions of
mental illness. - Interesting and challenging times lie ahead, as
we attempt to tackle identified areas of weakness
and need, if we are to empower this client group.
22
CONCLUSION Continued
- Need to develop method/database for recording
unmet needs, to build up picture of gaps in
service - The AVON will provide a starting point for
addressing quality issues and a spur to the
development of more adequate data - Highlight possible examples of good practice
- Looking at database
23
CONCLUSION Continued
- To empower clients to receive responsive or
relevant services - To develop services that more fully reflect the
needs and expectations of mental health service
users - To be effective clinical governance will require
data about the quality of care. This is a
starting point (although no direct conclusions)
24
. And Finally
Historically, services for disabled people have
been constructed upon the erroneous belief that
they are unable to assume responsibility for
their own individual needs. Therefore, logic
dictated that if individuals cannot assume
responsibility they cannot participate, if they
cannot participate they are excluded from main
stream society and discriminated against
(Woods, 1990)