Fulminant Hepatic Failure - PowerPoint PPT Presentation
1 / 31
Title:
Fulminant Hepatic Failure
Description:
Uncontrolled study. 75 patients with ALF and grade III encephalopathy ... Systematic review of liver support. Pascher et al Xenotransplantation 2002 9(5):309 ... – PowerPoint PPT presentation
Number of Views:1522
Avg rating:5.0/5.0
Title: Fulminant Hepatic Failure
1
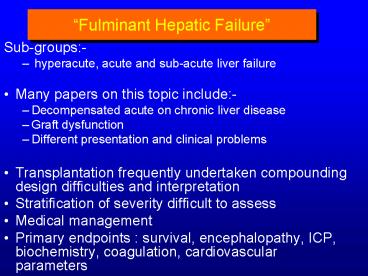
Fulminant Hepatic Failure
- Sub-groups-
- hyperacute, acute and sub-acute liver failure
- Many papers on this topic include-
- Decompensated acute on chronic liver disease
- Graft dysfunction
- Different presentation and clinical problems
- Transplantation frequently undertaken compounding
design difficulties and interpretation - Stratification of severity difficult to assess
- Medical management
- Primary endpoints survival, encephalopathy,
ICP, biochemistry, coagulation, cardiovascular
parameters
2
Hyper - acute liver failure Acute liver
failure Greatest risk of cerebral oedema, CVS
failure Greatest chance of spontaneous survival
Sub - acute liver failure Lowest risk of cerebral
oedema/encephalopathy Lowest chance of
spontaneous survival
3
Support of the failing liver
- Why
- improved outcome
- environment for regeneration and recovery
- support and bridge to transplantation
- Options
- Cell based therapies
- ELAD, BAL, BELS,Organ in a bucket..
- Dialysis methods
- Albumin dialysis (MARS, promethseus) Ash, CVVHF
- Plasmapheresis
- Needs to be
- Safe
- readily available and easily applied
- Clinically effective and cost effective
4
Haemoperfusion
Human Studies
5
- Human Studies
- Gimson AES et al Lancet 19822681-3
- Uncontrolled study
- 75 patients with ALF and grade III encephalopathy
- 10 hrs of charcoal haemoperfusion
- 65 survival in treated patients
- 15 survival in historical controls
- OGrady JG et al Gastroenterology 1988941186-92
- Controlled study
- 62 patients with ALF and grade IV encephalopathy
- No perfusion/ 10 hrs perfusion daily
- Survival 39.3 vs. 34.5 (non-significant)
- No survival benefit
6
- Biologic-DT randomised controlled study
Haemodiabsorption - Hughes RD et al, Int J Art Org199417(12)657-662,
Ellis AJ et al, - Int J Art Org 199922(1)27-34
- 10 patients with ALF 5 treated (5- 6 hour
treatments), 5 controls - Treated No change in ammonia, lactate, bile
acids, HE - Increased ACT, reduced fibrinogen, platelets
- Survival Treated 1/5 (20), Controls 3/5 (60)
- Retrospective study Aladag M Transplantation
Proceedings 36,203-5(2004) - 25 patients with FHF 12 liver dialysis
decision not to Rx based on - availability of machine or hepatologist choice
- Total plasma exchange undertaken to correct
coagulopathy - 50g 25 albumin added to prime for charcoal
haemodiabsorption - Rx grp acetaminophen 10, autoimmune 1 herbal rx
1 - Control grp acetaminophen 10, unknown 2, HBV 1
7
Mean treatment sessions 1.5 (1-3) of 4-5
hours Bilirubin 9.35 vs 5.66 mg/dl NH4 98 vs
113 µmol/l INR 1.88 vs 3 Treated grp 1 died,
2 OLT, 9 discharged home SOC grp 4 died, 2 OLT,
7 discharged home
8
MARS therapy 8 hour treatment or continuous
treatment
Other options- Albumin dialysis 8 hour
treatment standard filter 4500 ml buffer 1000
ml 20 albumin
9
- Novelli et al Liver 2002 22 suppl 2 43-7
- 34 patients 9 PNF, 9 ALF, 6 delayed graft
function, 10 AoCLD - Significant decrease in NH4 and Bilrubin, No
change in PT - 6/9 ALF underwent OLT (4 survivors) 3 survived
without OLT - Liver Transplant 2004101109
- 18 patients with alcoholic hepatitis MARS or
SMT over 7 days - Significant improvement in encephalopathy
- No change in renal function or creatinine
- No change in ammonia or cytokine levels (TNF,
IL-6, IL-10, IL-8) - No change in plasma malondialdehyde (MDA)
- Significant fall in bilirubin in MARS group
- Significant fall in N0x levels in MARS group
- MELD score decreased significantly in both groups
10
MARS and CVS and CNS parameters
- Schmidt et al Liver Transplantation 2003 9(3)
290-7, - Scand J Gastroenterology 200439(10)974
- FHF patients 8 Rx MARS, 6 cooled
- MAP 695 to 8311 mmHg plt0.001 No change with
cooling - CI 4.61.8 to 3.7 1.1 p0.0007 7 decrease with
cooling - HR 10521 to 8515 plt0.01 No change with cooling
- D02 621198 to 486141 plt0.05
- V02 14231 to 112 21 plt0.01 No change of
lactate or pH - 7 FHF, 5 AoCLD 20 decrease in total aa, No
change in BCAA - Fischers ratio increased 0.730.47 to 0.910.54
- Efflux of cerebral amino acids was not affected
- No change in CMR for any aa
11
MARS and Acute liver failure Awad et al
Surgery2001130354
- 5 patients ALF and 4 AoCLD HBV, Budd Chiari,
AIH, PNF Acetaminophen - 2 survived (1 OLT) 3 died All AoCLD died
- Factor VII 13.94.9 to 23.24.8 (p0.015)
- HES score 3.80.1 to 20.7 p0.02 ICP 373.9 to
13.32.8 p0.048
12
- MARS and ALF Isoniemi H et al Trans Proc 37,
1088(2005) - 49 patients with ALF overall survival 82 14
OLT, 26 med Rx - Toxic aetiology had better outcome median no Rx
3.1(1-9) - Hepatic encephalopathy 1.6 1.6 to 1 1.5
13
MARS post-operative liver failure Rittler et al
Liver Int 200424(2)136 Kellersman R Liver
200222suppl 256
- 5 patients treated post liver resection 1
survivor - Improvements seen in bilirubin, HE and renal
chemistry - 5 patients with post-op liver failure and MOF
- 13.41.9 treatments FFP and platelets support
- Significant fall in Bilirubin
- No falls in ammonia
- Worsening coagulation parameters (APTT)
- Increased transfusion requirements, bleeding
- Severe abdominal infection worsening
- APACHE II 151.4 to 282.7 - All patients died
14
(No Transcript)
15
- Zhou et al Artif Organs285 2004 Drug induced
liver failure Rx - MARS Rx in 14 patients grade I-III, 13
discharged,3 died DIC, 2 - subsequently died of variceal bleeding
- Significant decrease in NH4 (15760 to 9525)
bilirubin (680260 - to 392137) PT
- Gan et al World J Gastroenterol 2005 11(6)890
- Hepatocyte system vs plasma exchange vs control
in 30 patients - Survival 30, 20 and 0
16
Plasmapheresis
- Advantages
- Removes all molecules
- Substitutes plasma products
- coagulation factors
- Is well tolerated
- Improves HE, CMRgl and O2
- increases CPP and CBF
- No effect upon ICP,
- Increases MAP SVRI
- Decreases CI/DO2 but not VO2
- Increases splanchnic removal NH4
- Disadvantages
- Limited transport of water-soluble substances
- Unselective removal substances
- Requires donor plasma
Transport filtration/convection Membrane
plasma-filter Replacement donor plasma Toxins
all entire plasma phase
17
Whole liver perfusion Transplantation 2000
70(10)1472
- Human and porcine livers - continuous perfusion
until transplantation or withdrawal - 14 patients with 16 livers in 18 circuits
- 9 successfully bridged to transplantation
- ICP and CPP stabilized
- NH4 146 to 83 over 12 hours
- Maintained over 48 hours same for porcine or
human livers - Bilirubin decreased 385 to 198 over 12 hours
18
Systematic review of liver supportPascher et al
Xenotransplantation 2002 9(5)309
- Systematic review 1994-2000
- 198 patients - long term survival 28 (as per
standard of care) - Independent predictors of positive outcome
- Age lt 20 years plt0.029
- Coma lt III/IV plt0.003
- Perfusion time gt 10 hours plt0.024
- Use of human or baboon livers plt0.02
19
Use of discarded human livers in
bioreactorsGerlach JC Int J artif Organs 2002
25(10)1013Sauer et al Int J Artif Organs 2002
25(10) 1001 Busse et al, Arch Surg 1999 384588
- Bioreactor module with 3D-capillary structure
containing 1.8-4.0 x1010 (up to 500g) pig
hepatocytes. Kept perfused on stand-by for up to
3 weeks. - 20-25 of livers not used as transplants
- 54 human livers not used due to steatosis,
cirrhosis, fibrosis and other reasons - 36 reactors were produced of which 10 were used
to treat 8 patients - Treatment period 7 to 144 hours
- No adverse events reported
20
Porcine bioartificial liver - Amsterdam BALvan
de Kerkhove et al Int J Artif Organs
200225(10)950 Porcine radial flow bioreactor
Morsiani E et al Int J Artif Organs 2002
25(3)192
- Bioartificial liver - radial flow 3D high
density - 7 patients treated on 8 occasions
- Age 21 -56 years Grade III/IV HE
- Treated for 8 - 35 hours
- 6/7 proceeded to OLT
- 1/7 improved - no OLT required
- Plasmapheresis and subsequent exposure to cells
(230g) - 7 patients treated on 8 occasions
- HBV n3, primary non-function n3, 1 abdominal
trauma and liver surgery - 6/7 proceeded to OLT
- 1/7 recovered
- Improved encephalopathy, decreased ammonia,
decreased AST
21
ELAD in ALF Ellis et al, Hepatology 1996 24
1446-1451
Grp 1 17 possible recovery 7/9 S (Rx) vs 6/8
S(SoC) Grp 2 Tp criteria 7 listed 1/3 1/4
survived Worsening HE 7/12 SoC. 3/12 in ELAD
group
6
Lactate
5
4
3
mmol/l
Mean
SE, n-12
2
ELAD
Control
1
0
0
12
24
36
48
Perfusion time (h)
No difference for Bilirubin, AKBR, INR, factor
V, NH4 galactose clearance improved at 6 hours
22
New ELAD - 5 patients - all proceeded to Tp. (4
survived) Biocompatible MAP increased at 16
hrs. ammonia fell at 72 hrs increase in lactate
at 48 hrs. ICP and CPP stable Millis et al
Transplantation 200274 (12) 1735
23
Bioartificial Liver Rozga et al Ann Surg 1993
217502-9
- Hollow fibre cartridge
- 50 g pig hepatocytes on collagen coated
microcarriers - Incorporated into an extracorporeal circuit
- 2 charcoal columns
- heater
- oxygenator
- plasma resevoir
- Plasma (centrifugation) perfusion
- Applications of 6 to 7 hours
- Non-Randomised studies suggest benefit
24
BALArkadopoulos et al Int J Artif Organs
19982112781-787
23 patients with acute liver failure 17
underwent OLT mean period of 42 hours
support 5 recovered 1 died
Pre- Post- Bilirubin (mg/dl) 9.20.8 7.8
0.7 (plt0.001) Lactate 4.40.7 4.20.7
(NS) ICP 172 111 mmHg (Plt0.001) CPP 692
742 mmHg (P0.04) Ammonia 1598 13316 µmol/l
(plt0.001) PT (sec) 211 221 (NS)
25
Hepatassist in acute liver failureSamuel D
Transplantation 2002 73(2)257
- 13 patients with acute liver failure
- 3 not treated - 2 improved, 1 transplanted
- GCS 6.53.7 to 9.64.4 (plt0.02)
- related to volume of plasma exchange to BSA
- Decreased bilirubin (plt0.0005)
- 6 patients had transient haemodynamic instability
- 5 had bleeding complications
- 2 died post OLT 8 survived
26
Phase III study with BAL Demetriou et al Ann
Surg 2004239 660-670
27
Aetiology known (84)
Aetiology unknown (64)
- Co-variate time dependent proportional hazard
model of time to - account for impact of transplantation
- RR for BAL for all patients (171) 0.67 NS
- RR for FHF/SHF (148) was 0.56 p0.048
- Similar incidence of serious adverse events in
each group - No differences seen for neurological function
- Effect of multiple centres and variable management
28
Cell function and exposure
- Differing culture techniques to improve cell
function - Microgravity, 3 D systems, co-culture, Bio
engineering - Different culture and perfusion media Filippi J
Hepatol 2004 41599 - Effect of FHF sera unclear
- McCloskey Artif Organs 2002 26(4), Mitry Trans
Proceed 2005 372391 - Hyperacute rejection of porcine cells
- Van de Kerkhove J Hepatol 2005 42(4) 541-7
- Expression of galalpha(1-3)gal expressed at low
levels and see depletion of IgG and IgM antibody
after exposre to system - PERV infection
- DiNicuolo G 2005 Xenotransplantation
- Human plasma perfused through AMC BAL No
evidence PERV - 14 patients transient PERV DNA ive , cleared
by 2 weeks, no RNA ive
29
Systematic review JAMA 2003289 (2)217
Cochrane database 2004 (CD 003628)
- Of 528 references 12 randomised trials in 483
patients - 10 acute or AOC liver disease, 2 acute liver
failure - Recent trials not included
- Overall support systems had no effect on
mortality - compared with standard care (RR 0.65 CI
0.65-1.25) - 5 haemodiasorption, 2 MARS, 2 cellular and
remaining exchange techniques - Meta regression suggested that effect was
dependant on type of liver failure (p0.03) - In stratified meta analysis support systems may
decrease mortality in AOCL (33) but not in ALF
30
Assessment of severity assess and stratify
- Aetiology has significant impact on outcome
- Assessment must be bed side applicable and
reproducable - OGrady criteria acetaminophen and
nonacetaminophen - OGrady et al Gastroenterology 1989 Bernal
Hepatology 1998 271050 - Lactate Acetaminophen Bernal Lancet 2002359
- PO4, alpha feta protein Schmidt Hepatology 2002
36658 Hepatology 200541(1) - Clichy criteria factor V and encephalopathy
Similar predictability to KCH - criteria Pauwels J Hepatol 1993 17(1), Annand J
Hepatol 1997 26(1)62 - Liver volume and necrosis on biopsy Shakilao et
al Dig Dis Sci 200045(2)334 - MELD FHF definition MELD gt30
- Yantorno Liver Transplantation 200410C36
Wiesner Liver Transplantation 2004 10 (2) - Subsequently must track physiology in a
meaningful manner accounting - for medical management and natural history of
disease - SOFA and organ failure score
31
- Support systems are becoming more sophisticated
- Combining modular aspects
- BUT
- Well designed trials
- Appropriate stratification disease process,
aetiology, severity - Well defined end points
- SOC must be determined
- Must not forget the basics when enthused by new
machines - Fluids, CVS care, glucose control, sepsis,
feeding, neurological care - Avoid extrapolation to all diseases
- Coagulopathy, sepsis, drug clearance, DIC
- Need for well designed trials before general
application