Case 1 - PowerPoint PPT Presentation
1 / 37
Title:
Case 1
Description:
DM, CRI, dilated cardiomyopathy, CHF, COPD, gout, cirrhosis with ascites. Family Hx: ... PMHx: OSA, depression, gout. Social Hx: (-) tobacco/ETOH/IVDA. Meds: ... – PowerPoint PPT presentation
Number of Views:142
Avg rating:3.0/5.0
Title: Case 1
1
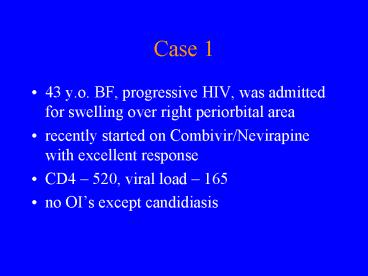
Case 1
- 43 y.o. BF, progressive HIV, was admitted for
swelling over right periorbital area - recently started on Combivir/Nevirapine with
excellent response - CD4 520, viral load 165
- no OIs except candidiasis
2
History
- 2 weeks PTA, fell and had minor abrasions over R
forehead ? papular eruptions over area ? lesions
started to become pruritic, oozing, and crusting
symptoms worse after washing with soap and water
used Neosporin - around the same time, remembers being bitten by
a bug over right lower eyelid - () new perfume use about 1 week PTA
3
History
- Reynolds Health Center diagnosed periorbital
cellulitis, given Augmentin - improved slightly at first, but later without
benefit - ID clinic 1/30 periorbital swelling, no visual
changes - admitted for IV antibiotics
4
History
- started on Cefazolin
- no improvement in 48 72 hours
- mild local itching and swelling, no pain
- (-) fever, () chills
- denied cutaneous exposure to allergens
- no similar previous episodes
5
History
- PMHx HIV, HCV, () chickenpox
- PSHx s/p hysterectomy
- Family Hx () CAD
- Social Hx () tobacco, ETOH, h/o IVDA
- Meds
- Combivir, Nevirapine, Cefazolin, Fluconazole
- Allergy sulfa ? rash
6
PE
- middle aged BF, NAD
- Temp 98.9 BP 109/63 HR 73
- well-demarcated area of dry, scaly rash over R
eye, R forehead, R cheek () cervical,
submandibular lymphadenopathy - rest of exam unremarkable
7
Labs
- WBC 4.1
- 54 segs
- BUN 14
- Creatinine 1.0
- AST 63
- ALT 40
8
(No Transcript)
9
(No Transcript)
10
(No Transcript)
11
Hospital Course
- ID Consult
- unlikely infectious
- d/c Cefazolin
- Derm consult
- Dermatology Consult
- likely allergic contact dermatitis
- Desowen topically BID
- no soap to face
12
Case 2
- 63 y.o. WM, diabetic, multiple medical problems
had new onset nausea/vomiting since 1/18 - ER visit _at_ Wilkes showed acute on chronic renal
failure CxR showed widened mediastinum ? CT
chest showed pneumomediastinum ? WFUBMC (2/1)
13
History
- gastrograffin swallow ? esophageal perforation ?
OR - mediastinal abscess ? drained
- R thoracotomy, intercostal muscle flap
- esophageal tear closure, gastrostomy, feeding
jejunostomy - empirically started on zosyn/cipro
14
History
- PMHx
- DM, CRI, dilated cardiomyopathy, CHF, COPD, gout,
cirrhosis with ascites - Family Hx
- non-contributory
- Social Hx
- heavy ETOH use in past
- recently quit tobacco
15
History
- Medications
- Zosyn, Cipro, ranitidine, prns
- Timentin at OSH
- Allergy
- sulfa
16
PE
- Temp 99 BP 107/71 HR 100
- sedated, intubated
- lungs clear bilaterally
- () thoracotomy scar, chest tube, PEG tube/
J-tube - wounds clean, (-) discharge
- Otherwise unremarkable
17
Labs
- WBC 11.4 (from 25.4)
- 10 bands
- Creatinine 3.4
- CxR
- L lung effusion, LLL ATX/infiltrate
- widened superior mediastinum
- CT/gastrograffin study as mentioned
18
Microbiology Data
- Sputum culture (-)
- Urine culture (-)
- Blood culture (-) (2 of 2)
- OR swab
- 2 yeast, 1 GPC on culture
- 1 yeast, 2 WBC on Gram stain
19
- Andersen et al 1992
- prevalence study of esophageal candida
colonization in Danish population - 164 subjects stratified according to /- COPD
- questionnaire probing for symptoms of esophageal
disease - PFTs, EGD, LES pressure measurement
- surface material from esophageal plaques,
erosions, exudates, or normal-appearing mucosa
obtained plated on agar plate - considered () if at least 50 colonies C.
albicans grew within 72 hours
20
- Andersen et al 1992
- prevalence ranges from 12 25
- overall estimate in Danish population 20
- no statistically significant difference in
prevalence between following subject groups - benign esophageal disease
- esophagitis
- GERD
- COPD
- no significant clinical correlation between
esophageal symptoms () C. albicans
21
- Bauer et al 1996
- 2 case reports of invasive candidiasis
complicating Boerhaave Syndrome - Risk factors for secondary fungal infection
- preexistent Candida colonization
- incomplete mediastinal drainage
- broad-spectrum antibacterial therapy
- prolonged ICU stay
22
- Candida as a cause of mediastinitis very rare,
accounting for 5 - Clancy et al 1997
- review of 9 cases, all s/p thoracic surgery, 1 as
complication of esophageal leak - median time to disease onset of 11 days
- clinical manifestations
- purulent drainage from sternum (56)
- fever, sternal instability, chest wall erythema
(44) - shock (33)
- sternal click (22)
- resp. distress, subcutaneous emphysema, wound
dehiscence, and sternal tenderness (11)
23
- Clancy et al 1997
- 89 had Candida isolated in pure culture
- all specimens from mediastinum () Candida
- () blood cultures 44
- () sternal bone cultures 44
- () pleural fluid 22
- () pericardial fluid 22
- () urine culture 22
- () thrombus culture 22
- () wound site culture 11
- () hardware 11
24
- Clancy et al 1997
- Overall mortality 56 80 (4/5) of which
directly attributable to candidal mediastinitis - clinical manifestations not distinguishable from
bacterial mediastinitis - optimal therapy still unclear
- aggressive surgical debridement with antifungal
therapy is the preferred approach - duration of antifungal unclear, but at least 6
weeks recommended
25
Case 3
- 51 y.o. WM, OSA presented to OSH with
- 2 3 week h/o polyuria, polydipsia, anorexia,
weight loss, bloody stool, vomiting, confusion - work-up revealed glucose of 1,467 AG 29
- admitted with HONC, ARF, fever of 102
- reportedly (-) head CT
- became hypotensive ? pressors
- Temp ? to 107, started on CTX ? further clinical
decline ? transferred to WFUBMC
26
History
- PMHx OSA, depression, gout
- Social Hx (-) tobacco/ETOH/IVDA
- Meds none
- Allergy NKDA
27
Hospital Course
- On arrival, BP 68/40, temp 101.3
- aggressively hydrated, electrolytes replaced
- started on levophed/dopamine gtt
- started on heparin gtt (troponin 7)
- empirically started on CTX/EES/ACV
- CT head, LP, EEG performed
- ID consulted for MS changes
28
PE
- Temp 102.7 BP 110/72 HR 103
- overweight middle ages WM
- intubated, sedated
- PERRL, anicteric
- lungs clear, tachycardic, RRR, (-) m/r/g
- soft abdomen, () BS
- (-) skin lesions/rash
29
Labs
- WBC 24.8 ?12.7
- 85 segs, 2 bands
- BUN/Creatinine 39/5.5
- Na 160 ? 146 CO2 13
- CK 4,080 (peaked _at_ 5,728)
- lactic acid 4.4 ? 1.3
- UA () ketones, 5 8 WBC, 50 RBC
30
Labs
- LP
- OP 36 CSF red and cloudy
- WBC 150 RBC 22,100
- 76 segs
- glucose 118 protein 94
- Crypto Ag (-) HSV-PCR (-)
- Gram stain (-) organism, 2 WBC
- bacterial Ag (-)
31
Labs
- Blood urine cultures (-) to date
- CxR NAD
- Head CT
- possible Chiari I malformation, mild cerebral
edema, () infarct over R posterior limb of
internal capsule
32
Extreme Pyrexia Simon 1976, JAMA 2362419-21
- 28 cases of extreme pyrexia, patients with temps
between 41.1 42.2 C (106 108 F) - retrospective study in MGH, 1970-75
- ages 6 74, mean 39
- 23 males, 5 females
- grouped into 4 categories based on etiologic
diagnosis
33
Extreme Pyrexia
- Group 1 11 patients (39)
- infection as sole cause of fever
- 7 px with GNR sepsis 1 had TB lymphoma
- 1 px with Staphylococcal line sepsis
- 1 px with pneumonia
- 1 px with pyelonephritis, blood cultures (-)
- 1 px with malaria
34
Extreme Pyrexia
- Group 2 9 patients (34)
- infection impaired thermoregulation as cause
- 4 severe burn patients with extensive occlusive
dressings sepsis (3 GNR, 1 fungal) - 3 paraplegia/quadriplegia infection (2 pyelo, 1
mediastinal abscess) - 1 massive ICH pneumonia
- 1 viral encephalitis
35
Extreme Pyrexia
- Group 3 5 patients (18)
- thermoregulatory failure as cause
- 3 with heat stroke (11)
- 2 with massive ICH
- Group 4 3 patients (11)
- etiology unclear
- ? JRA
- ? viral infection
- ? drug/pyrogen reaction
36
Extreme Pyrexia
- 18/28 (64) occurred June September
- ? influence from ambient temperature
- 8/28 (29) died
- only 2/28 (7) died from severe pyrexia
- mortality otherwise dependent on underlying dx
- no change in neurological function could be
attributed to the fever itself in any of the cases
37
Extreme Pyrexia
- height of fever not helpful in establishing
etiologic cause - thermoregulatory failure
- excessive heat production
- thyroid storm malignant hyperthermia
- impaired heat dissipation
- heat stroke, burn patients with extensive
occlusive dressings - disordered hypothalamic function