Types of Bones - PowerPoint PPT Presentation
1 / 94
Title: Types of Bones
1
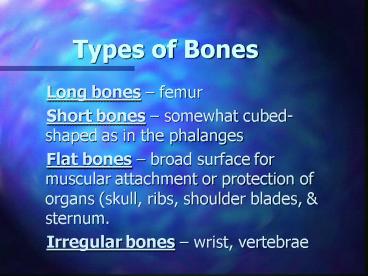
Types of Bones
- Long bones femur
- Short bones somewhat cubed- shaped
as in the phalanges - Flat bones broad surface for muscular
attachment or protection of organs (skull, ribs,
shoulder blades, sternum. - Irregular bones wrist, vertebrae
2
Functions of Bones
- Support protect body tissues and organs
- Provides the skeletal framework of the body
- Provides movement through the attachment of
muscles - Storehouse for minerals CA 99 makeup
of bones PO4 90 Po4 - Production of blood cells) which takes place in
the bone marrow
3
Diarthrodial/Synovial Joints
- - Ball socket i.e. shoulder hip which
permits movement in any direction - - Hinge i.e. elbow movement along one plane
allows flexion extension - - Condylar functions like a hinge joint but
can - rotate slightly
4
Synovial Joint Capsule
- Fibrous connective tissue covers the ends of
bone. Ligaments and tendons reinforce the joint
capsule - Bundles of rich, white fibrous tissue are
supplied with nerves. Nerves are sensitive to
rate and direction of motion, compression,
tension, vibration and pain - Blood vessels, and lymphatic vessels.
5
Skeletal Muscles
- Primary Function
- Provides voluntary movement
- Maintains posture
- Body Movement contraction relaxation
6
Skeletal Muscles
- Points of Attachment
- Point of Origin attachment of muscle to a more
stationary bone - Point of insertions attachment to a more
movable bone
7
Head to Toe Assessment
- Health History
- Musculoskeletal disorders
- Nutritional status
- Pain History
- ADLs, endurance, assistive devices
- Medications prescription and OTC
8
Assessment Skills
- Inspection symmetry, body alignment, function,
skin changes, swelling, deformity, contractures,
gait, non-verbal indication of pain - Palpation Skin temperature, swelling, nodules,
masses, Crepitus - Joint Structure ROM
- Muscle mass strength (atrophy, flaccidly,
spasticity, paralysis)
9
Connective Tissue Disorders
- Rheumatoid Arthritis
- Osteoarthritis
- Lupus Erythematous
- Gout
10
Rheumatoid Arthritis
- Autoimmune connective tissue disorder
characterized by inflammatory destructive changes
in the joints - Systemic disease Inflammatory changes can
affect skin, heart, lungs, eyes, blood vessels
nerves
11
Etiology of Rheumatoid Arthritis
- Autoimmune theory Normal antibodies become
autoantibodies (RH Factors) and attack the
tissue. - Genetic Factor 2-3 times with family Hx
- Virus Epstein-Barr
- Stressful events
12
Stages of Joint Deterioration
- Stage 1 Initiation - Some changes in the
synovial lining no loss of functional capacity - Stage 2 Immune Response Joint swells
thickens. Functional capacity impaired - Stage 3 Inflammatory Progressive involvement of
blood vessels. Limited ADL - Stage 4 Destructive Granulation tissue hardens
(Pannus). Leads to ankylosis. Confined to bed or
wheel chair
13
Assessment Data
- Subjective
- - Stiffness especially in a.m. or after
- inactivity
- - Proximal joint pain in the fingers
- - Fatigue, weakness, 2-3 weight loss, low
grade fever
14
Assessment Data
- Objective Manifestations
- - Swollen, reddened, warm joints
- - Weak hand grasp
- - Deformities (late stages)
- Swan Neck
- Ulnar Drift
- Boutonnière (buttonhole)
- Rheumatoid Nodules
- Vasculitis, Sjogrens Syndrome
15
Diagnostic Tests
- Blood Tests
- - Rheumatoid Factor
- - Antinuclear Antibody Titer
- - Erythrocyte Sedimentation Rate
- - CBC WBC
16
Diagnostic Tests
- Radiographic determines cartilage erosion, joint
space narrowing, bone cysts - - Arthrography- x-ray with contrast medium
- - Arthroscopy endoscopic exam of joint
- - Arthrocentesis needle aspiration of
- synovial fluid
17
Nursing CareArthroscopy Post-procedure
- Assess Neurovascular status (Sx. of
thrombophlebitis) - Monitor for bleeding or leakage at site
- Assess for pain, edema, redness
- Ice for swelling, mild analgesic pain
18
Pain Management
- Prescribed Drug Therapy on timely basis
- Rest periods
- Warm shower, hot packs
- Avoid sudden, jarring of joint
- Warn clients about quacks (miracle cures)
19
Impaired Physical Mobility
- Exercise joint, but not beyond pain
- Positioning body alignment
- Support joints for optimal function
- Assistive Devices proper fit instruction
20
Self-care Deficit
- Routine that includes pacing activities
- Encourage sleep routine
- PT for conditioning
- Occupational Therapy Assistive devices
21
Drug Therapy
- Salicylates (ASA)
- NSAIDs (Advil, Indocin, Toradol, naprosyn)
- Side effects/Precautions
- Tinnitus, GI distress, prolonged bleeding. Give
with food, milk. Avoid anti-coagulants
22
Drug Therapy
- Side effects/Precautions
- GI (do not crush enteric coated) give after
meals or with food - Dizziness, Diarrhea, headache, rash
23
Drug Therapy
- Glucocorticoids (dexamethasone, hydrocortisone,
prednisone.) - Side Effects/Precautions
- Depression, euphoria, anorexia, nausea,
- weight gain, bruising. Taper dosage when
discontinuing.
24
Drug Therapy
- Slow-acting Antirmalirial drugs (plaquenil)
- Side Effects/Precautions
- Retinal edema, GI disturbance
- Toxic Gold Salts (solganol, myochrysine)
- Side Effects/Precautions
- Dizziness, flushing, metallic taste, skin rash
assess CBC UA prior to administration
25
Drug Therapy
- Cytoxic Drugs (Methotrexate, Imuran, Cytoxan)
- Side Effects/Precautions
- Pneumocystis Carni pneumonia, mouth sores, bone
marrow suppression, hepatotoxicity
26
Degenerative Joint Disease(Osteoarthritis)
- Non-inflammatory disease of the weight bearing
joints (hips, knees, spine, hands) - Incidence in post-menopausal women
- Risk Factors age, obesity, overuse of joints,
trauma (fractures, sports injuries)
27
Osteoarthritis
- Pathophysiology Articular cartilage becomes
yellow opaque, joint space narrows, bone spurs
(osteophyte), cysts - Symptoms Joint pain / diminishes on rest
crepitus (grating sensation) Joint enlargement,
Herberdens nodes, Bouchards nodules, decrease
ROM, joint effusion
28
Osteoarthritis
- Diagnostic Tests X-rays of joints indicates
narrowing of joint spaces CT Scan MRI of
spine Bone Scan - Differential features of RA DJD
- OVERHEAD Table 24-1
29
Osteoarthritis
- Medical Management
- Drug therapy for pain (NSAIDs), muscle
relaxants(Flexeril), injection of cortisone - Rest immobilization with splint, brace, sleep
(8 hours/night) - Position of joints to maintain alignment avoid
contractures - Heat hot packs, PT diathermy
- Exercise walking, water aerobics
30
Osteoarthritis
- Surgical Management
- Hemiarthroplasty one part of a joint is
replaced, i.e. head of femur - Total Hip replacement Head of femur the
acetabulum replaced - Total Knee replacement both articular surfaces
of the knee replaced - Interphalangeal joint replacement
31
Total Hip Replacement
- Preoperative Care Skin preparation, IV
antibiotics, education re nature of prosthesis,
mobility restrictions, exercises - Types of Prosthesis
- - Cemented 10 year life
- - Uncemented bone growth occurs into the
metallic surfaces within 6-12 weeks
32
THR - Postoperative
- Pain control
- Wound drain assessment
- Neurovascular Assessment
- Activity bed rest with abduction splint or
pillow, OOB with PT (NO hip flexion 90) weight
bearing dependent on type of prosthesis - Use of walker crutches - cane
33
THR - Potential Complication
- Thromboembolism
- Subluxation - Hip Dislocation
- Neurovascular Compromise
- Hemorrhage
34
THR Hip Precautions
- Avoid hip flexion 90
- Avoid low, soft chairs
- Avoid excessive trunk flexion in reaching
- Maintain hip adduction
- No leg crossing at knee
- Use raised toilet seat
35
Total Knee Replacement
- Preoperative Care similar to THR
- Postoperative Care
- - Pain control
- - Wound drain assessment
- - Neurovascular Assessment
- - Elevate leg on Pillow for comfort
- - Head of bed elevated for comfort
- - Continuous Passive Motion Machine
36
TKR - Potential Complications
- DVT pulmonary emboli
- Prosthetic Dislocation
- Infection
37
Lupus Erythematous
- Definition Autoimmune disease involving diffuse
inflammatory changes in vascular connective
tissue - Pathophysiology Antigen-antibody interactions
results in deposits of immune complexes in
tissues cells that damage the organs and or
blood vessels
38
Discoid Lupus
- Cutaneous manifestations butterfly
- rash on face
- Risk Factors Sun exposure intensifies
- Treatment Cortisone creams, sun screens 30
SPF, avoid sun at peak hours
39
Systemic Lupus
- Organs affected Heart, lungs, kidney, Brain,
blood vessels, joints - Systemic symptoms Fatigue, myalgia, joint pain,
low grade fever, anorexia - System specific symptoms Tachycardia, chest
pain, poteinuria, hip knee necrosis, psychosis,
seizures
40
Laboratory Tests of SLE
- Skin biopsy scrapings of skin cells
- Immune tests RF, ANA, Sed Rate
- CBC (pancytopenia), Sed Rate, Cardiac Liver
Enzymes
41
Pharmacological Management Lupus
- NSAIDS
- Cortico-steroids
- Immunosuppresive Agents
42
Nursing Care - Lupus
- Pain Management
- Encourage rest periods
- Decrease protein in diet (kidney involvement) and
sodium restriction (fluid retention) - Referral Local National Lupus Foundation
43
Potential Complications Lupus Erythematous
- Vasculitis
- Cardiopulmonary pericarditis, pleural effusion
- CNS psychosis, seizures, peripheral
neuropathies - Avascular Necrosis
44
Gout
- Definition Systemic disease involving pain
inflammation of joints due to urate crystal
deposits - Pathophysiology Inbalance of purine metabolism
kidney function - Incidence Middle aged men
45
Types of Gout
- Primary Inherited defect in purine metabolism
- Secondary Disease i.e renal, diuretic therapy
chemotherapeutic agents
46
Clinical Manifestations of Gout
- Asymptomatic phase Elevated Uric Acid
- Acute Phase Sustained elevated Uric Acid
causing extremely painful, swollen, and reddened
joint - Chronic Phase Urate crystal deposits appear in
cartilage, synovial membranes, tendons, soft
tissues
47
Drug Therapy - Gout
- Acute Phase Colchicine, NSAIDS
- Chronic Phase Allopurinol (Benemid)
- Colbenemid
- Avoid aspirin diuretics
48
Diet Therapy - Gout
- Low purine (avoid organ meats, shellfish, oily
fish with bones - Avoid Alcohol
- Increase fluid intake to 3,000 cc/day
- High alkaline ash foods citrus fruits and
juices, certain dairy products
49
Other Connective Tissue Disorders
- Polymyalgia Rheumatica
- Anklosing Spongylitis (Marie-Strümpell Disease)
- Sjögrens syndrome
- Lymes Disease
- Fibromyalgia
50
Osteoporosis
- Types
- Primary - Bone loss related to loss of estrogen
in menopausal women and low testosterone levels
in men - Secondary Bone loss related to disease process
(hyperthyroidism, renal failure, GI malabsorption
problems
51
Pathophysiology Bone Remodeling
- Resorption Worn out bone cells are removed by
bone-resorbing cells called osteoclasts - Formation New bone is laid down by bone-forming
cells called osteoclasts
52
Incidence/Risk FactorsOsteoporosis
- Age
- Race
- Gender
- Life Style
- Diet
- Heredity
53
Prevention of Osteoporosis
- Exercise weight bearing types
- Diet modifications
- Calcium intake OTC i.e. Tums, Oscal, Calcium
carbonate, Dietary supplement
54
Clinical ManifestationsOsteoporosis
- Height loss
- Vertebral deformities
- Restricted movement
- Back pain
- Fractures
55
Diagnostic TestsOsteoporosis
- Laboratory serum calcium, Vitamin D,
phosphorus, alkaline phosphatase - Radiological X-ray, CT Scan, MRI
- - Dual energy x-ray absorptiometry
56
Medical ManagementOsteoporosis
- Drug Therapy
- Estrogen replacement Premarin
- Calcium supplements
- Bone resorption inhibitor Fosamax
- Vitamin D
57
Nursing ManagementOsteoporosis
- High Risk for Injury Prevention of falls and
fractures - - safe environment
- (non-skid slippers, shoes, clean spills, avoid
scatter rugs, lighting, access to items for ADL,
hand rails, Avoiding lifting heavy objects, use
of walker, cane.)
58
Nursing ManagementOsteoporosis
- Impaired Physical Mobility
- Increase mobility to level of independence in
ADL - Interventions
- - Physical therapy program (strengthening
weight bearing exercises) - - Occupational Therapy (Adaptive Devices)
59
Nursing ManagementOsteoporosis
- Pain Management - Reduce alleviate pain
- Interventions
- - Drug Therapy - opiod, non-opiod Analgesics,
muscle relaxants, Anti-inflammatory agents - Use of heat
- Orthotic devices braces, splints
60
Other Metabolic Degenerative Bone Disorders
- Osteomalcia
- Pagets Disease
- Herniated Nucleus Pulposus
- - Laminectomy
- - Spinal Fusions
61
Fractures
- Definition Interruption in normal bone
continuity, which is accompanied by soft tissue
injury - Classification
- - Simple or closed
- - Open or compound
62
Fracture Patterns
- Oblique Line of Fx. Angled
- Transverse Across the bone
- Longitudinal Length of bone
- Spiral Twisting or rotation of bone
- Comminuted broken in 2 places
- Impacted Fragments driven into each other
- Displaced or Avulsed torn away by a ligament or
tendon
63
Classification by Anatomical Location
- Humerus
- Tibia, Fibula
- Pelvis
- Hip
- Skull
- Mandible
- Ribs
- Vertebrae
64
Stages of Bone Healing
- Hematoma
- Granulation
- Callus Formation
- Osteoblastic Proliferation
- Bone Remodeling
- Complete Healing
65
Bone Healing Problems
- Delayed Union - 6 months to a year
- Nonunion -
- Malunion Bone healed in state of deformity
66
Assessment of Fractures
- Subjective Data History, complaints of pain,
loss of sensation, movement - Objective Data Warmth, edema, ecchymosis,
neurovascular impairment, splinting, anxiety, fear
67
Emergency Care
- Inspect area
- Control bleeding
- Immobilize/splint
- Prevent shock
- Transport safely to ER
68
Nursing Diagnoses
- Acute Pain
- Risk for Neurovascular Dysfunction
- Risk for Infection
- Altered Mobility
- Activity Intolerance
69
Complications of Fractures
- Shock
- Neurovascular Compromise
- DVT Pulmonary Emboli
- Aseptic Necrosis
- Acute Compartment Syndrome
- Fat Embolism Syndrome
- Osteomyelitis
70
Shock
- Etiology Hemorrhage into damaged tissues,
especially thorax, pelvis, extremities - Treatment Control bleeding and restore blood
volume
71
Neurovascular Compromise
- Etiology Damage to nerves from fragments of
bone, pressure from casts, splints, traction - Treatment 6 Ps Pain, Pulslessness,
Paresthesia, Pallor, Paralysis, Poikothermia
72
Fat Embolism Syndrome
- Etiology Release of particles of fat into the
blood stream from the yellow marrow at site of
injury - Risk Factors Fx. of long bones, multiple fx.,
high serum glucose or cholesterol level
73
DVT Pulmonary Emboli
- Etiology Immobility, trauma, surgery
- Risk Factors Incidence in fractures of the lower
extremities Smoking, obesity, Heart Disease - Treatment Anticoagulants
74
Avascular Necrosis
- Etiology Loss of blood supply to bone
- Risk Factors Hip fractures or any fracture where
this bone displacement - Treatment Surgical joint replacement
75
Compartment Syndrome
- Etiology Massive compromise in circulation from
external (Tight, bulky dressings, casts)
internal (blood fluid) - Treatment Immediately loosen any tight
dressings MD can bivalve cast - Surgery Decompression fasciotomy for edema and
bleeding
76
Osteomyelitis
- Acute infection in another part of the body
invades bone tissue or occurs from penetrating
trauma - Chronic Infection persists especially in a
patient with compromised circulation
77
Medical Management of Fractures
- Closed Reduction immobilization Manual
traction to align the bone - External Fixation Percutaneous placement of
pins implanted into bone - - Kronner 4-Barr Compression Frame
- - Hex-Fix External device for tibial fractures
- - Halo Traction Cervical spinal fractures
78
Nursing Care External Fixation
- Teach patient patient to grasp frame when moving,
rather than limb - Frequent observation neurovascular assessments
- Pin Care Note symptoms of infection
- Assess for loosening or shifting of devices
79
Casts
- Purpose Immobilze, correct deformity, allow
early mobility, provide support protection - Types Plaster of Paris Fiberglass
80
Plaster Cast Care
- Instruct that cast will feel warm
- Handle cast with palms of hands
- Turn client q 1-2 hours for drying
- Elevate on pillow î than heart
- Pedal rough edges with moleskin
- Inspect q 4-8 hours drainage, cracking, odor,
alignment fit
81
Cast Complications
- Circulatory impairment
- Peripheral nerve damage
- Impaired skin integrity
- Pneumonia, DVT, Constipation
- Compartment Syndrome
- Cast Syndrome Body cast
- Fracture blisters
82
Traction
- Definition Pulling force that is applied to part
of an extremity while a counter traction pulls in
the opposite direction - Purpose Reduce Fracture, immobilize, decrease
pain muscle spasm, correct deformities, stretch
tight muscles
83
Types of Traction
- Continuous or Running Bucks, Russell
- Circumferential Pelvic
- Cervical
- Suspension or Balanced Thomas Ring
- Skeletal Steinmann pins, Kirschner wires,
Crutchfield tongs
84
Nursing Assessment
- Equipment weights, pulleys, ropes, Balkan
frame - Mobility
- Skin integrity
- Neurovascular
- Gastrointestinal
- Urinary
85
Fractured Hip
- Incidence Prevalent women 65 200,000
annually by age 80 1 in 5 - Risk Factors Falls, osteoporosis, age related
changes in balance
86
Anatomy of Hip
- Head of femur
- Acetabulum
- Femoral neck
- Greater trochanter
- Lesser or sub-trochanter
87
Types of Hip Fractures
- Femoral Neck displaced, impacted, comminuted
- Intertrochanteric (Intracapsular, Extracapsular)
- Subtrochanteric
88
Signs Symptoms of Hip Fractures
- Pain hip or thigh
- Adduction, external rotation
- Shortening of leg
- Inability to move or bear weight
89
Surgical Intervention
- Total Hip Arthroplasty
- - Cemented allows full weight bearing
- - Uncemented Full weight bearing not
permitted for 6-8 weeks - ORIF Intramedullay rods, plates, compression
screws allows early ambulation
90
Post-operative Care - ORIF
- Bedrest 1st day OOB with walker
- HOB î 35 - 40
- Avoid hip flexion 90
- Trochanter roll for hip alignment
- Pillow splint when turning (per MD)
- Isometric exercises
- Pain control narcotic analgesics
91
Complications ORIF
- DVT, PE
- Hemorrhage
- Infection
- Subluxation or dislocation
92
Carpal Tunnel Syndrome
- Definition compression of the medial nerve in
the wrist - Etiology Repetitive motions, wear tear,
Fracture of wrist - Symptoms Pain, paresthesia, difficulty in
grasping
93
Diagnostic Tests CTS
- Phalens wrist flexed back to back results in
paresthesia 60 seconds - Tinels Tapping over the median nerve pain,
tingling, numbness or inflating a BP cuff will
result in same SX. - X-ray
- EMG
94
Interventions CTS
- Non-invasive wrist support, immobilization with
splint, frequent breaks, cushion grippers on
pencils pens, Rest, Ice, Heat,
Anti-inflammatory agents - Invasive Cortisone Injections, Surgery