OPTIMA: Optimal Timing of PCI in Unstable Angina
1 / 25
Title:
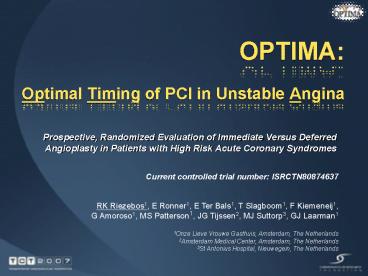
OPTIMA: Optimal Timing of PCI in Unstable Angina
Description:
Prospective, Randomized Evaluation of Immediate Versus Deferred Angioplasty in ... there is no need to rush to PCI in non-refractory high risk NSTE-ACS patients ... –
Number of Views:258
Avg rating:3.0/5.0
Title: OPTIMA: Optimal Timing of PCI in Unstable Angina
1
OPTIMA Optimal Timing of PCI in Unstable Angina
- Prospective, Randomized Evaluation of Immediate
Versus Deferred Angioplasty in Patients with High
Risk Acute Coronary Syndromes
Current controlled trial number ISRCTN80874637
RK Riezebos1, E Ronner1, E Ter Bals1, T
Slagboom1, F Kiemeneij1, G Amoroso1, MS
Patterson1, JG Tijssen2, MJ Suttorp3, GJ Laarman1
1Onze Lieve Vrouwe Gasthuis, Amsterdam, The
Netherlands 2Amsterdam Medical Center, Amsterdam,
The Netherlands 3St Antonius Hospital,
Nieuwegein, The Netherlands
2
Disclosure Statement of Financial Interest
- I, Robert Riezebos DO NOT have a financial
interest/arrangement or affiliation with one or
more organizations that could be perceived as a
real or apparent conflict of interest in the
context of the subject of this presentation.
3
Introduction
- Current guidelines recommend an early invasive
strategy in high risk NSTE-ACS - The precise timing of early PCI is controversial.
- Immediate PCI may prevent (spontaneous) cardiac
events - Deferred PCI may lead to less peri-procedural
complications
4
OPTIMA trial
- Optimal timing of PCI in unstable angina
- To compare immediate with 2448 hours deferred
PCI in the early invasive management of NSTE-ACS - Hypothesis In high risk NSTE-ACS immediate PCI
reduces cardiac events
5
Patient selection
- Screening at hospital admission
- Chest pain at rest lt 6 hours
- At least one of the following
- Cardiac troponin T gt 0.01 ng/l
- ST depression gt 0.1 mV in 2 contiguous leads
- History of coronary artery disease
- 2 or more risk factors for coronary artery
disease - No clinical indication for urgent PCI
- Written informed consent (before angiography)
6
Angiographic inclusion
- Immediate angiography
- Culprit lesion amenable to PCI
- Angiographic exclusions
- CABG preferred treatment
- CTO culprit
- ISR culprit
7
Randomized treatments
- Randomization in cathlab after angiography
- Immediate PCI
- Ad hoc PCI of culprit lesion
- Deferred PCI
- PCI of culprit lesion 24-48 hours later
- Triple antiplatelet therapy
- Abciximab, clopidogrel and aspirin
8
Primary endpoint
- Composite of
- Death
- Non fatal MI
- Unplanned revascularization
- within 30 days
9
Sample size
- Event rate in control group 30,
- Immediate PCI 35 relative risk reduction
- Power 80, a 0.05 (two-sided)
- 2 x 300 randomized patients
- After enrollment of 251 patients interim analysis
was performed - 142 patients were randomized
10
Flow chart
11
Baseline demographics
12
Baseline risk factors
13
Baseline characteristics ACS
14
Time from randomization to PCI
15
PCI characteristics
16
Medication
17
Primary endpoint at 30 days
18
Primary endpoint at 30 days
19
Clinical events at 30 days
20
MI at 30 days
21
Adjusted composite endpoint (negative CKMB at
randomization)
22
Infarct size during initial hospitalization
peak CKMB
Plt0.01
CKMB (median) 9.8 4.9 (ng/L)
23
Other clinical events at 30 days
24
Limitations
- Limited sample size due to early discontinuation
of patient inclusion - Unexpected results opposite to hypothesis
- The play of chance
25
Conclusions
- Immediate PCI increased the rate of
periprocedural MI compared to a cooling down
strategy of deferred PCI - The results of the study suggest that there is no
need to rush to PCI in non-refractory high risk
NSTE-ACS patients





![Optimizing Fish Passage Barrier Removal Using Mixed Integer Linear Programming [Preliminary Report]](https://s3.amazonaws.com/images.powershow.com/A1256673324bwtEl.th0.jpg?_=20150806063)
























